General
- Can be done via 3 following approaches
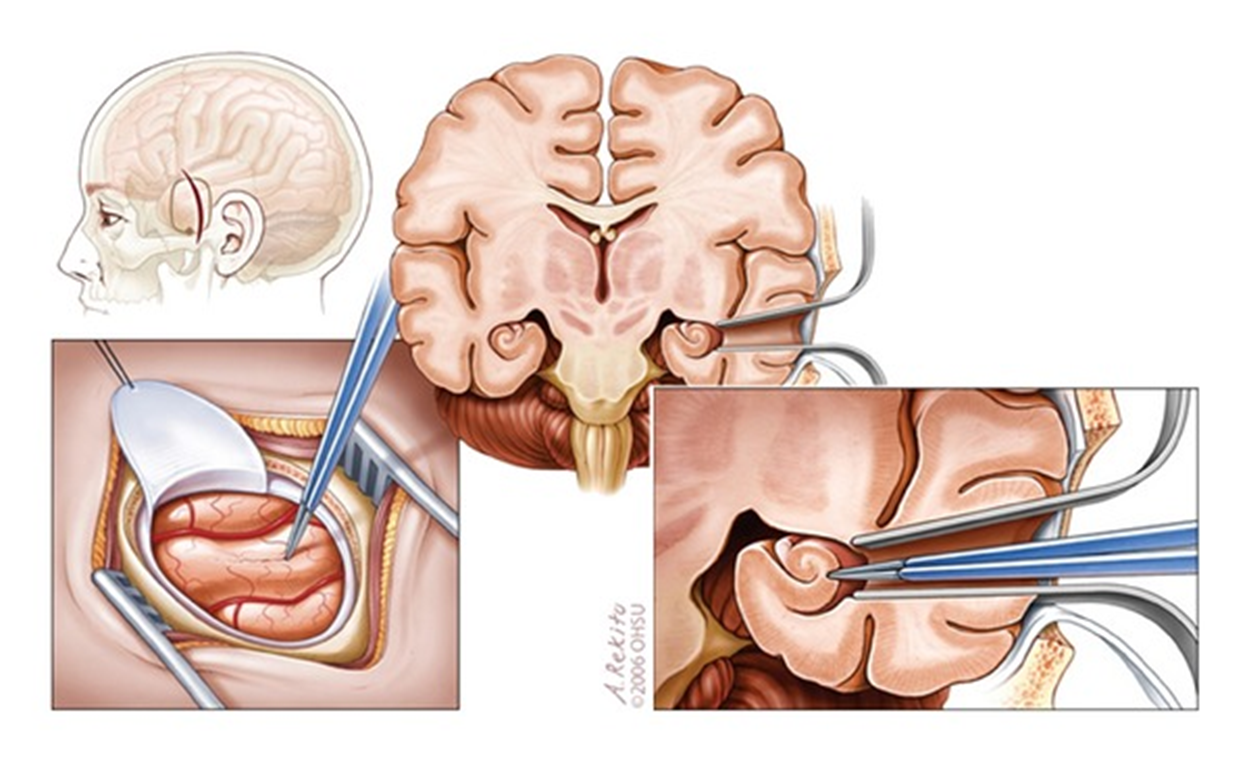
Subtemporal approach
- Advantage
- Avoids injury to Meyer's loop → visual field defects
- Fewer neuropsychological sequelae
- But data are limited
- Disadvantages
- Requiring excessive retraction of the temporal lobe → injury vein of Labbe
- May require removal of the zygomatic process.
Transcortical-Middle temporal gyrus
- Positioning
- Brainlab
- Supine
- 3-pin fixation
- Rotated 90 degrees to the opposite side, and parallel to the floor.
- Dura opened and flapped inferiorly.
- Brainlab identification of the cortical incision in the middle temporal gyrus that is 2.5–3.0 cm behind the tip of the temporal lobe and in an area free of cortical vessels
- Corticotomy is generally 2–2.5 cm in length.
- Guided by neuronavigation, dissection is performed toward the temporal horn until the temporal horn is entered
- Two self-retaining brain retractors are placed to provide an optimal view of the intraventricular anatomy, and key anatomical structures are identified.
- The parahippocampal gyrus is resected beginning with subpial resection of the uncus and then advancing medially and posteriorly, with frequent confirmation of location using neuronavigation and care to preserve the mesial pial border.
- With resection of the anterior uncus, the incisura is visualized, and superiorly the internal carotid artery and third nerve can be seen through the pia.
- The choroidal fissure is identified. Care must be taken to insure that the dissection is not carried superior to the choroidal fissure.
- The hippocampus is then mobilized laterally and resected beginning anteriorly, with care to preserve the anterior choroidal artery, and carried posteriorly to the level of the tectal plate. Once the hippocampal resection is completed, the cerebral peduncle and anterior choroidal artery are visualised through the pia.
- Neuronavigation is used to confirm the completeness of the resection, and careful hemostasis is obtained.
- Postop
- Neurological exam
- Head CT
- Care is taken to continue antiepileptic medications. Following overnight observation in a neurological intensive care unit, the patient completes a typically 3-4-day postoperative hospital stay before discharge to home.
Translyvian-Inferior limiting sulcus of the insula
- Head of the patient is positioned so that sylvian fissure is parallel to the surgeon's view.
- Completely splitting the sylvian fissure as posteriorly as possible
- Inferior circular sulcus of the insula is entered → through the temporal stem → roof of the temporal horn, at the level of or just posterior to the limen insulae, → the temporal horn is reached.
- Through the inferior circular sulcus of insula, the entry point through the roof of the temporal horn is located on average 8 mm from the lateral aspect of the lateral geniculate body;
- No demarcation between the lateral geniculate body of the thalamus and the roof of the temporal horn, since the major component of the roof of the temporal horn is constituted by the meyer’s loop or geniculocalcarine fascicle, which originates from the lateral geniculate body.
- A more medial removal of the roof of the temporal horn to improve visualization of the choroidal fissure should be performed with caution as it can damage the thalamus and lateral geniculate body
- Once the temporal horn has been entered, the same procedure through the choroidal fissure is performed.
- At the stage of uncal removal through the transsylvian approach, the same landmarks as described earlier for the Amygdalaectomy can be adopted.
- = removal of the uncus (Amydala is within uncus)
- In the subpial anterior temporal lobectomy, in which the uncus is approached subpially from its lateral aspect, the arteries constitute the most important anatomic landmarks for this purpose.
- Anteromedial surface of the uncus is related to the internal carotid artery and the proximal half of the Ml segment of the middle cerebral artery;
- Inferior portion of the vertex of the uncus is related to the oculomotor nerve;
- Inferior portions of the posteromedial surface of the uncus are related to the P2A segment of PCA turning around the crus cerebri
- Superior portions of the posteromedial surface of the uncus are related to the posterior part of the cisternal segment of the anterior choroidal artery just before entering the temporal horn through the choroidal fissure.
- Superiorly, there is no clear demarcation between the amygdala and the globus pallidus.
- Subpial resection of the uncus can be deemed adequate when the following vascular landmarks is visualised through the Pia:
- Anterior and anterior-medially:
- The visualisation of ICA and the proximal segment of the MCA indicates that the anteromedial surface of the uncus has been removed;
- Inferiorly:
- Visualisation of the oculomotor nerve
- Posterior medially:
- P2A segment of the posterior cerebral artery
- Superiorly:
- Optic tract: Hard to visualise
- Posterior portion of cisternal segment of the anterior choroidal artery, as it runs under the optic tract;
- Initial portion of the cisternal segment of the anterior choroidal artery does not always follow the superior portion of the uncus, whereas its posterior portion, close to the inferior choroidal point, is constantly related to the superior portion of the posteromedial surface of the uncus.
- Carotid-choroidal line:
- A line is traced from the bifurcation of the internal carotid artery or the proximal segment of Ml to the inferior choroidal point
- Almost the entire uncus will stay below this line.
- It is not advisable to cross this line superiorly because of the risk of invading the globus pallidus
- Intraventricularly, the posterior portion of the amygdala is the prominence on the roof of the temporal horn immediately anterior to the inferior choroidal point, which passes below this line, and it can be removed until this line is established,
- Posterosuperior:
- The inferior choroidal point.
- The highest point of the uncus
Amygdalectomy
Images
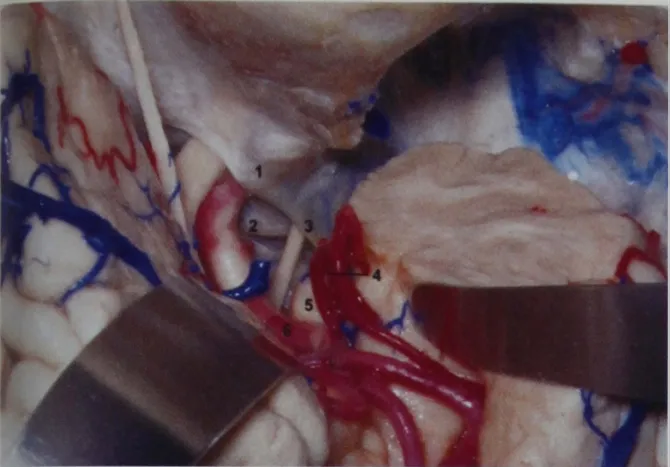
Transsylvian exposure.
A coronal cut has been performed at the temporal pole demonstrating that there is no amygdala located at that level.
1, Anterior clinoid process;
2, Posterior clinoid process;
3, Oculomotor nerve and tentorial edge;
4, Rhinal sulcus (beneath the temporal branches of the middle cerebral artery);
5, Anteromedial surface and apex of the uncus;
6, M1 segment of the middle cerebral artery.
A coronal cut has been performed at the temporal pole demonstrating that there is no amygdala located at that level.
1, Anterior clinoid process;
2, Posterior clinoid process;
3, Oculomotor nerve and tentorial edge;
4, Rhinal sulcus (beneath the temporal branches of the middle cerebral artery);
5, Anteromedial surface and apex of the uncus;
6, M1 segment of the middle cerebral artery.
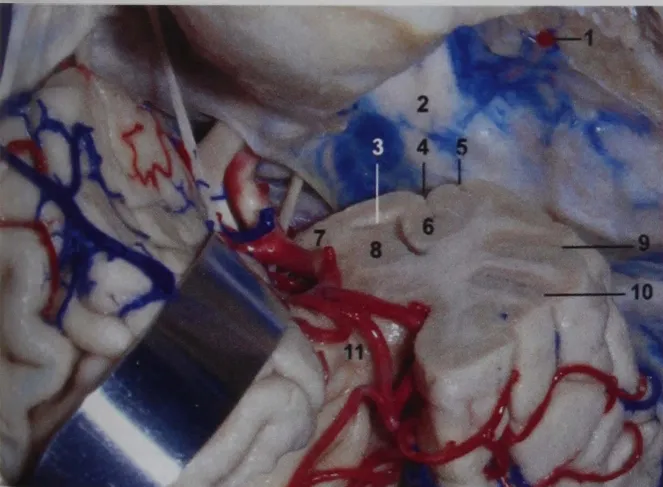
Another coronal cut was performed on the temporal lobe at the level of the middle cerebral artery. Note that the collateral sulcus is located laterally to the tentorial edge, and the amygdala bulges inferiorly toward the head of the hippocampus.
1, Middle meningeal artery;
2, V2 and V3 (trigeminal nerve);
3, Temporal horn;
4, Collateral sulcus;
5, Occipito-temporal sulcus;
6, Collateral eminence;
7, Apex of the uncus;
8, Amygdala;
9, Inferior temporal sulcus;
10, Middle temporal gyrus;
11, Limen insulae.
1, Middle meningeal artery;
2, V2 and V3 (trigeminal nerve);
3, Temporal horn;
4, Collateral sulcus;
5, Occipito-temporal sulcus;
6, Collateral eminence;
7, Apex of the uncus;
8, Amygdala;
9, Inferior temporal sulcus;
10, Middle temporal gyrus;
11, Limen insulae.
Pros
- Avoids injury to the temporal neocortex and underlying white matter that is traversed in the transcortical approach and allows en bloc resections of the mesial temporal structures.
Cons
- More technically difficult
- Allows limited surgical exposure → risk of transaction of the temporal stem,
- Poses a greater potential risk of vascular injury or vasospasm
- Though this has rarely been reported in large surgical series