General
- Praxis = the ability to perform skilled movements.
- Praxis requires both (both are independent of each other but both are needed for normal functioning)
- Conceptual system
- Conceptual knowledge of tool functions and actions
- Eg: the purpose of a screwdriver
- Deficit causes conceptual apraxia
- Test
- Naming of actions,
- Naming of tools,
- Specification of tool use
- For example,
- ‘‘What would you use a toothbrush for ?’’,
- ‘‘Which is the correct movement for brushing teeth?’’ with the examiner miming both the target action and distractors
- Production system
- Sensorimotor action programmes concerned with the generation and control of movement
- Eg: the ability to move a limb through space in the correct direction and with appropriate speed
- Deficit causes idea-motor apraxia
- Test
- Hand and finger position imitation
- Execution of familiar action sequences
- For example,
- ‘‘Fold a piece of paper, place in envelope and seal the envelope’’
- Execution of single familiar actions
- Verbal command
- ‘‘Show me how you would use a toothbrush’’,
- Imitation of examiner’s mime,
- Ability to pantomime usage while looking at the tool
- ‘‘Pretend you have this in your hand. Show me how you would use it’’
- Actual tool use ‘‘Take this in your hand and show me how you would use it’’
Ask patients: Show me how you would…. (if they cannot understand or follow commands test by imitation
Type | Praxis Exam Task | ㅤ |
Buccofacial | Blow out a match | ㅤ |
ㅤ | Lick lips | ㅤ |
ㅤ | Cough | ㅤ |
ㅤ | Sip through a straw | ㅤ |
Limb | Gestures | Wave goodbye |
ㅤ | ㅤ | Beckon "come here" |
ㅤ | ㅤ | Salute, like a soldier |
ㅤ | ㅤ | Hitch a lift |
ㅤ | Comb hair | Brush teeth |
ㅤ | ㅤ | Use scissors |
ㅤ | ㅤ | Hammer a nail |
ㅤ | ㅤ | Object use |
- Normal motor function
- Prefrontal cortex (SMA + others)
- Provides the will and intention to do a task,
- Left fronto-parietal systems activates motor engrams (for example, the pattern and sequence of movements needed to light a match) in Premotor cortex
- Fed down to the primary motor cortex
- Corticospinal tracts to muscle
- Modulation from cerebellum and basal ganglia.
- Need to exclude Disorders that might interfere with the production of skilled movements
- Sensory loss or more elemental motor disorders:
- Weakness, tremors, dystonia, chorea, ballismus, athetosis, myoclonus, ataxia, or seizures or
- Severe cognitive, memory, motivational, or attentional disorders.
- Although the presence of these disorders does not preclude apraxia, before making this diagnosis the clinician should be certain that these behavioral disorders do not fully account for the patient's inability to perform skilled acts
- Due to
- Developmental
- Neurological dysfunction.
Loss of motor function
- Dyspraxia
- Difficulty performing motor acts which cannot be accountable by lack of understanding of the task, weakness, or proprioceptive loss.
- Partial loss
- Many patients with dyspraxia are unaware of their deficits, thus the examiner should specifically enquire from the patient and caregiver as to how the patient manages activities of daily living such as brushing teeth, combing hair, using kitchen utensils, etc.
- Dyspraxia is frequently missed by clinicians, and may then be detected by occupational therapists or physiotherapists—for example, when seeing patients recovering from stroke.
- Apraxia
- Complete loss
- Can even occur in the presence of an additional deficit such as hemiparesis, but to qualify as apraxia, the examiner must be confident that the apparent difficulty performing the motor act cannot be explained by the hemiparesis alone
- Mechanism
- It is thought that it results from loss of motor engrams or a disconnection between praxis systems.
- Causes
- Stroke
- Neurodegenerative disease
- Alzheimer’s disease
- Corticobasal degeneration
- Progressive isolated limb apraxia
- Subdivisions of apraxia
- Orobuccal apraxia
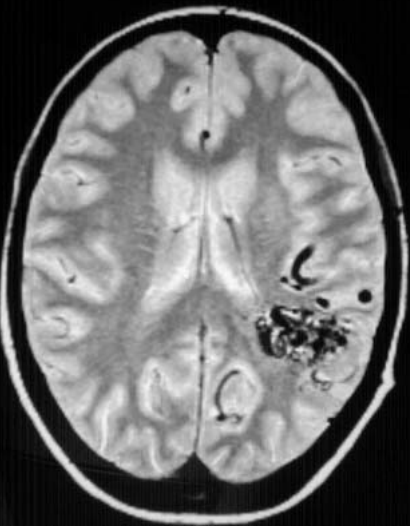
- Damage to
- Insular
- Left inferior frontal lesions
- Limb apraxia:
- Damage to
- Left parietal
- Left frontal premotor
- 6 subtypes
- Clinical presentation
- A loss of deftness including the ability to make finely graded, precise, individual, but coordinated finger movements.
- The patient may have difficulty picking up a straight pin from the top of a desk using a pincher grasp of the thumb and forefinger.
- Usually affects the hand that is contralateral to a hemispheric lesion.
- Test
- Rapid Finger Oscillation Test
- Grooved Pegboard Test
- Timed coin rotation between thumb, index, and middle fingers
- Pathophysiology
- Damage to
- Corticospinal system
- Convexity premotor cortex
- Conceptual system error
- Defects in mechanical knowledge needed to select tools and objects.
- Clinical presentation
- Unable to recall the types of actions associated with specific tools, utensils, or objects (tool-object action knowledge)
- Eg: when asked to demonstrate the use of a screwdriver by either pantomiming or using the actual tool, the patient may pantomime a hammering movement or use the screwdriver as if it were a hammer.
- Unable to recall which specific tool is associated with a specific object (tool-object association knowledge).
- Eg: when shown a partially driven nail, they may select a screwdriver rather than a hammer from an array of tools.
- This conceptual defect may also be in the verbal domain: When a tool is shown to a patient, the patient may be able to name it, but when asked to name or point to a tool when its function is described, he or she might be unable to perform correctly.
- Unable to describe function of tools
- Unable to choose appropriate substitute for tools
- Using a screw driver as a hammer rather than a wrench to drive a nail
- Unable to create simple tools
- Pathophysiology
- Temporoparietal junction is integral to the mediation of conceptual knowledge.
- Contralateral to the preferred hand.
- Recommended tasks include
- Gesture to holding and seeing tools,
- Association tools with objects, and
- Demonstration of mechanical knowledge.
- Production system error
- Clinical presentation
- Make the most errors when asked to pantomime transitive acts to verbal command, and their performance typically improves with imitation.
- When they use tools or implements, their performance may improve even further, but it often remains impaired.
- Pts make primarily spatial and temporal production errors.
- Spatial errors include errors of
- Posture (or internal configuration)
- Cutting with a scissor: pt uses body part as the tool (a form of postural error) despite asking pt not to use body part (finger) as a tool
- Spatial movement
- Cutting an imaginary bread: make the correct core movement (e.g., twisting, pounding, cutting), but their limb movements through space are often incorrect
- Joint movements are not well coordinated, the patient may make primarily chopping or stabbing movements.
- Do not demonstrate a smooth sinusoidal hand speed when performing cyclic movements such as cutting with a knife.
- Spatial orientation
- Cutting an imaginary paper in odd planes rather than the horizontal plane
- Tests include
- Performing transitive movements to verbal command (pantomime to command),
- Imitating the examiner performing transitive movements,
- Performing transitive movements with actual tools or implements
- Discriminating between well-performed and incorrectly performed transitive gestures.
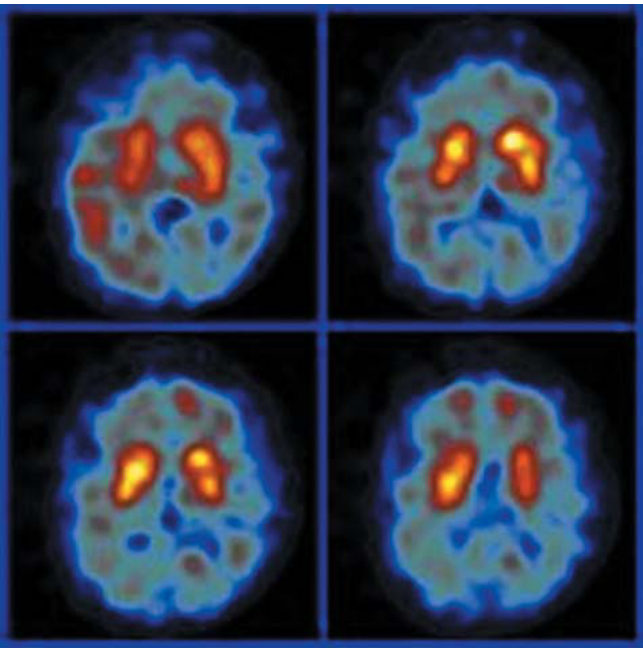
- Pathophysiology
- Contralateral to dominant hand
- Damage
- Corpus callosum
- Patients with apraxia from callosal lesions usually have unilateral apraxia (the nonpreferred hand).
- Lesions here allows patients to discriminate well from incorrectly performed gestures
- Inferior parietal lobe
- Lesions here does not allow patients to discriminate well from incorrectly performed gestures
- Supplementary motor area
- Lesions here allows patients to discriminate well from incorrectly performed gestures
- Basal ganglia
- Hemispheric white matter
- Unable to pantomine with one sensory input (verbal) but able to pantomine normally with other sensory inputs (visual, tactile)
- Verbal is the most common sensory deficit (hence sometimes called verbal disassociation apraxia)
- Test
- Pantomime to visual or tactile stimuli,
- Pantomime to verbal commands,
- Imitation,
- Use of actual objects
- Pathophysiology
- Callosal lesion
- The praxias are controlled in the Left premotor and parietal areas → callosal lesion blocks communication between Left and right hemisphere → Right motor cortex cannot get info from left premotor and parietal areas. → unable to produce movements → ideamotor apraxia of left hand. Normal praxia of right hand
- The praxias and language /speech are controlled in the Left hemisphere → synthesized Praxia + Verbal input cannot get access to the right hemisphere → Idea motor apraxia of Left hand but not right.
- Patients can perform imitation and use of actual objects correctly because Visual input can enter the right hemisphere directly from the right Visual cortex → movement representations stored in their right hemisphere can be activated by visual input.
- Complex
- Left-handed patients with right hemisphere lesion
- IMA without aphasia.
- Right hemisphere (because now the right hemispshere is dominant): stores movement → Bilateral idea motor apraxia
- Left hemisphere: Stores language (70% of left-handed people) → not aphasic
- Left-handed patients with right hemisphere lesion + callosal lesion
- Combined of the following causes Left arm Disassociation apraxia + Right arm idea motor apraxia: Disassociation apraxia is more severe than idea motor apraxia as idea motor apraxia still allows some movement although abnormal. However disassociation apraxia has no movement at all.
- Right hemisphere (because now the right hemispshere is dominant): stores movement → Bilateral idea motor apraxia
- Callosal lesion doesn't allow Left hemisphere (stores language) to communicate with right hemisphere (stores movement) → verbal pantomine cannot be understood by right hemisphere → Disassociation apraxia of their left arm.
- Left hemisphere: Stores language (70% of left-handed people) → not aphasic
- Because patient was similar to patients with conduction aphasia who repeat poorly, hence it is termed this disorder conduction apraxia.
- Clinical presentation
- More apraxic to imitating than pantomiming to command
- Test: imitation to command.
- Pathophysiology
- Normal:
- When a patient sees a pantomine, patient's visual system could access movement representations, also termed praxicons, and these activated movement representations could access semantic-conceptual representations.
- Decoding a gesture might require accessing different movement representations (input praxicon) than those important in programming an action (output praxicon).
- Conduction aphasia:
- A disconnection of the input and output lexicons
- Conduction apraxia:
- A disconnection between the input and output praxicons
- Damage
- The lesions that induce conduction aphasia are usually in the supramarginal gyrus or Wernicke's area,
- But the location of lesions that induce conduction apraxia is unknown.
- The inability to carry out a series of acts or formulate an ideational plan
- Clinical presentation
- Patients have difficulty sequencing the acts in the proper order.
- Erroneous use of ideational apraxia. For example,
- Disassociation apraxia.
- Ideamotor apraxia:
- Patients with Ideamotor Apraxia usually improve when using tools and objects, some researches used ideational apraxia as patients who made errors with the use of tools and objects
- Although the inability to use actual tools and objects may be associated with a conceptual disorder, a severe production disorder (IMA) may also impair object use.
- Conceptual apraxia:
- The term ideational apraxia has also been used to describe patients who make conceptual errors
- Test
- Assessment of ability to perform multistep tasks
- Pathophysiology
- Frontal lobe dysfunction is often associated with time order processing deficits.
- Pick (1905) noted that most patients with this type of ideational apraxia have a degenerative dementia.
Limb kinetic apraxia (fine motor) | Conceptual apraxia (knowledge) | Ideomotor apraxia (moving) | Disassociation apraxia (disconnect) | Conduction apraxia (repeat) | Ideational apraxia (Sq) | |
Definition | A loss of deftness including the ability to make finely graded, precise, individual, but coordinated finger movements. | Conceptual system error where there is defects in mechanical knowledge needed to select tools and objects. | A production system error where they are not able to generate and control movement | Unable to pantomine with one sensory input (verbal) but able to pantomine normally with other sensory inputs (visual, tactile) | More apraxic to imitating than pantomiming to command | The inability to carry out a series of acts or formulate an ideational plan |
Presentation | •Nothing to do with movement but all to do with knowledge •Defects in mechanical knowledge needed to select tools and objects. | •Abnormal movement but nevertheless some movement is present •Verbal pantomine worse than visual pantomine. •Using tools or implements improves deficits | No movement at all | |||
Test | •Rapid Finger Oscillation Test •Grooved Pegboard Test •Timed coin rotation between thumb, index, and middle fingers | •Pantomime to command •Cutting a piece of paper | •Pantomime to visual or tactile stimuli •Pantomime to verbal commands •Imitation •Use of actual objects | Imitation to command. | Assessment of ability to perform multistep tasks | |
Damage | •Corticospinal system •Convexity premotor cortex | -Temporoparietal junction -Contralateral to dominant hand | •Corpus callosum (contralateral to dominant hand) •Inferior parietal lobe •Supplementary motor area •Basal ganglia •Supramarginal gyrus of the Non dominant parietal lobe | •Callosal lesion (contralateral to dominant hand) | Unknown | Frontal lobe dysfunction |
Limb kinetic or melokinetic, apraxia
Conceptual
Ideomotor
Disassociation
Conduction
Ideational apraxia
Gain of motor function
- Damage
- Prefrontal cortex
- Normally
- Prefrontal cortex exerts an inhibitory effect on the ability of perceptual input to result in motor response
- Allowing humans to carve an autonomous path in the world rather than be a slave to our environment.
- Pathology
- Prefrontal pathology can remove this inhibition, leading to a compulsion to act on the surroundings (that is, environment dependency syndrome or forced utilisation behaviour).
- Eg: a patient in a room with hammer, nails, and a picture, will hammer a nail into the wall and hang the picture. If asked why he did that, he will say ‘‘I assume from the items being there that this is what you wanted me to do’’
- Premotor cortex
- Motor cortex
- Eg: focal motor seizures
- Alien hand syndrome
- Often associated with apraxia, in this disorder the limb may perform movements not under volitional control, as if it has a will of its own.
- Severe alien hand on one side may result in intermanual rivalry, such as the anarchic hand trying to throttle the patient while the other hand under volitional control tries to fend it off, but such circumstances are rare and tend to occur transiently in the context of acute cerebrovascular disease.
- Damage
- Progressive isolated alien limb is essentially pathognomonic of corticobasal degeneration
Complete assessment: Combined test for all
- Place a pen on the table with the cap close
- Ask patient to name it and what it is used for
- Test for conceptual apraxia
- Ask patient to pantomine using a scissor
- Ideomotor apraxia
- Can do partial pantomine that is abnormal
- Dissociation apraxia
- Completely unable to do so
- Ask patient to copy me writing and then ask patient verbally to pantomine writing
- Conduction apraxia
- Ask patient to pick up pen using finger and thumb
- Test for limb kinetic apraxia
- Ask patient to uncap pen and place the cap behind the pen and write his name and then putting pen down
- Ideational apraxia