General
- The veins are a capacitance network
- 75% of blood pool at any given time is situated in the veins. (for both spine and brain)
- The intradural (intrinsic and extrinsic cord) and extradural (epidural plexus, paravertebral) systems are highly redundant and therefore fail only under extreme circumstances.
- The weak link, and therefore site of pathology, are the transdural connections — radiculomedullary and bridging veins.
- These veins are relatively limited, and have no effective alternative pathway for venous egress through the dural cover.
- Their paucity and failure is as much responsible for symptoms of dural arteriovenous fistula as the shunt-related pathologic inflow.
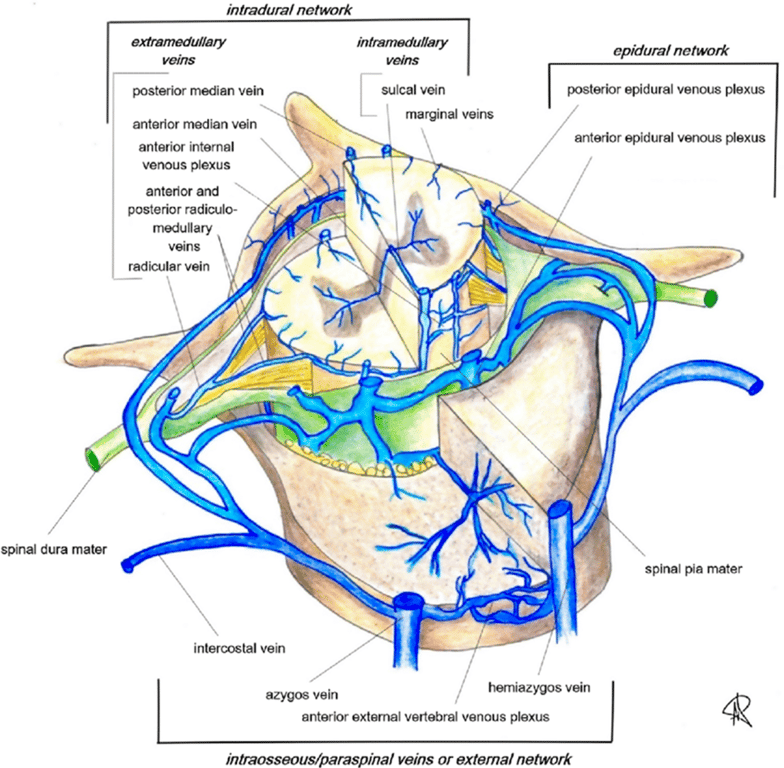
Spinal venous system can be divided into four systems/components:
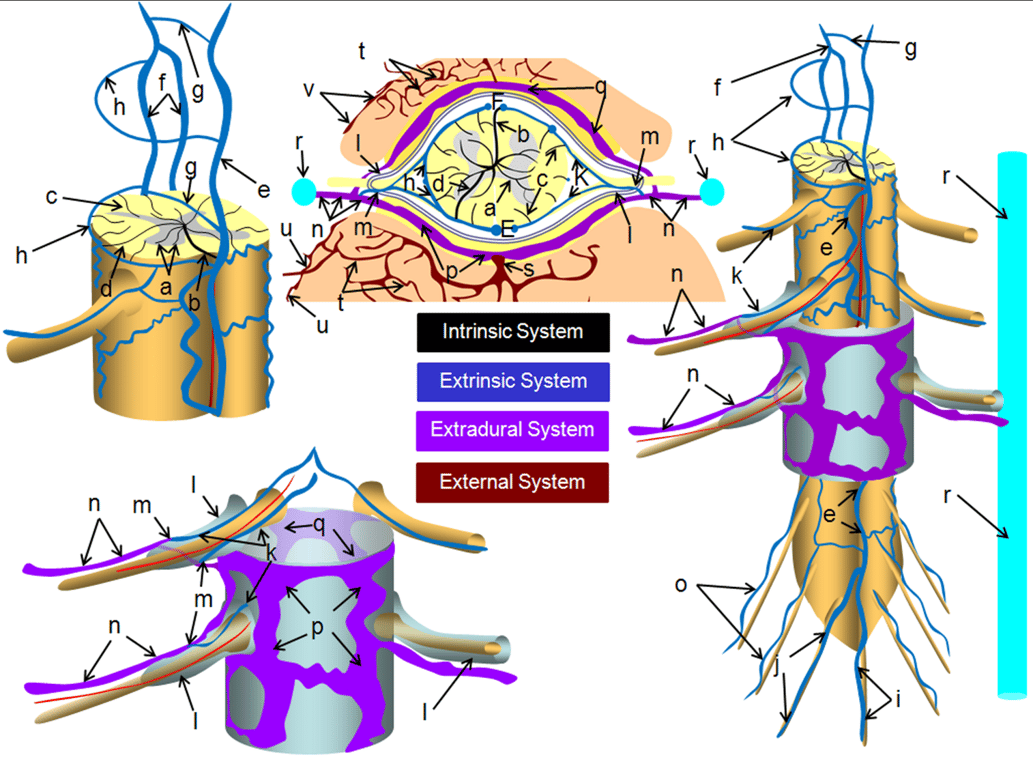
Category | Description | Vessels | Best imaging modality: Cone-beam computed tomography (CBCT) |
Intrinsic | intramedullary / intrinsic cord veins | a –centripetal network of veins, predominantly draining the gray matter into: b – central (sulcal) veins of the intrinsic system; c – peripheral (radial, a.k.a. marginal) centrifugal veins of the intrinsic system; d – venous anastomosis between the centripetal and centrifugal systems; | Commercially available noninvasive imaging has essentially no role. Intrinsic cord veins are below MRI resolution. Catheter angio — combination of 2D-DSA and CBCT are the best we have. We only see veins of the arterial territory we inject. |
Extrinsic | cord surface veins and the radicular / bridging veins which allow venous outflow to traverse the dura | e – anterior (ventral) median vein; f – posterior (dorsal) median vein; g – transmedullary anastomosis between dorsal and ventral median venous systems; h – extrinsic surface anastomosis between dorsal and ventral median veins; i – vein of filum terminale; j – dominant radicular vein of the cauda equina; k – radicular vein (this is the weak link between the cord venous system and the extradural space) aka radiculomedullary vein or Medullary vein; m – shallow angle of radicular vein piercing the dura of the nerve root sleeve; o – radicular veins of the cauda equina; | Cord Surface Veins (anterior/ventral and posterior/dorsal) veins are inconsistently seen on MRI. •Sometimes too well, raising possibility of a fistula. •Mostly not well enough. Well seen when injecting dominant artery (Adamkiewicz) by angio and CBCT. Bridging and radicular veins can be seen surprisingly well on high-res T2. Well seen on CBCT and angio if large enough artery is injected. |
Extradural | epidural plexi and drainage into the bony spinal canal outside dura | n – intervertebral vein; p – anterior epidural (a.k.a. ventral intrinsic) venous plexus; q – posterior epidural (a.k.a. dorsal intrinsic) venous plexus; | Can be seen well enough on MR/CT, especially when congested. Phlebograms are excellent, and more often done now for CSF-venous fistulas. |
External | osseous, paravertebral, etc — anything outside the epidural space | s – basivertebral vein, draining the intravertebral body venous plexus (t); u – anterior extrinsic venous plexus surrounding the surface of the vertebral body; v – posterior extrinsic venous plexus on the surface of the lamina /posterior elements, also participating in drainage of the paraspinal muscles | MR/CT can be good. Catheter angio may be limited by unopacified inflow. |
- Epidural venous plexus
- Aka: Batson’s venous plexus
- extends from foramen magnum to the sacrum,
- Is a series of highly interconnected venous “lakes.”
- These connections are so extensive that the whole plexus can become part of an alternative conduit of venous blood from the lower extremities to the superior vena cava in cases of inferior vena cava obstruction
- The epidural venous plexus is highly redundant craniocaudally. So much so that these two disease are relatively asymptomatic
- Extradural Epidural AVF
- Extra-spinal AVMs (Parkes-Weber Syndrome, for example) have their AVM venous drainage conducted into the epidural venous plexus
- The epidural veins are only a part of the whole “Plexus” which also recruits paraspinal veins.
- It is also extensively connected with paraspinal veins outside of the spinal canal via the foraminal veins
- The foraminal veins across every foramen which is not stuffed, crushed, or otherwise obliterated by disks and osteophytes.
- These veins are well-seen with modern MRI imaging, especially on T2, as they are outlined by neural foraminal fat.