General
- Represents the gold standard of surgical management of temporal lobe epilepsy.
- Traditional surgical approach
Pros
- Good surgical exposure to allow complete resection of mesial structures
- Relatively low morbidity
- Permits pathological examination of en bloc specimens.
Pre op work up
For assessing language dominance in epilepsy patients via:
- Clinical presentation
- Neuropsychological assessment
- fMRI
- While functional MRI and/or magnetoencephalography may aid in language lateralisation
Important to work up because mesial temporal structures
- Especially the hippocampal formation, are critical for the formation of new memories.
- Both sides are involved in memory consolidation,
- Left verbal memories
- Right visuospatial (nonverbal) memories.
- Removal of the mesial temporal structures in a temporal lobectomy may lead to memory decline.
- Many patients with temporal lobe epilepsy have bilateral disease, hence a unilateral temporal lobectomy in a patient with poor function on the contralateral side could have catastrophic results, such as an amnestic syndrome.
Important structures to look out for
- Awake intraoperative cortical stimulation producing speech arrest to map critical language regions can be used as a guide to tailor the extent of resection of the dominant temporal lobe.
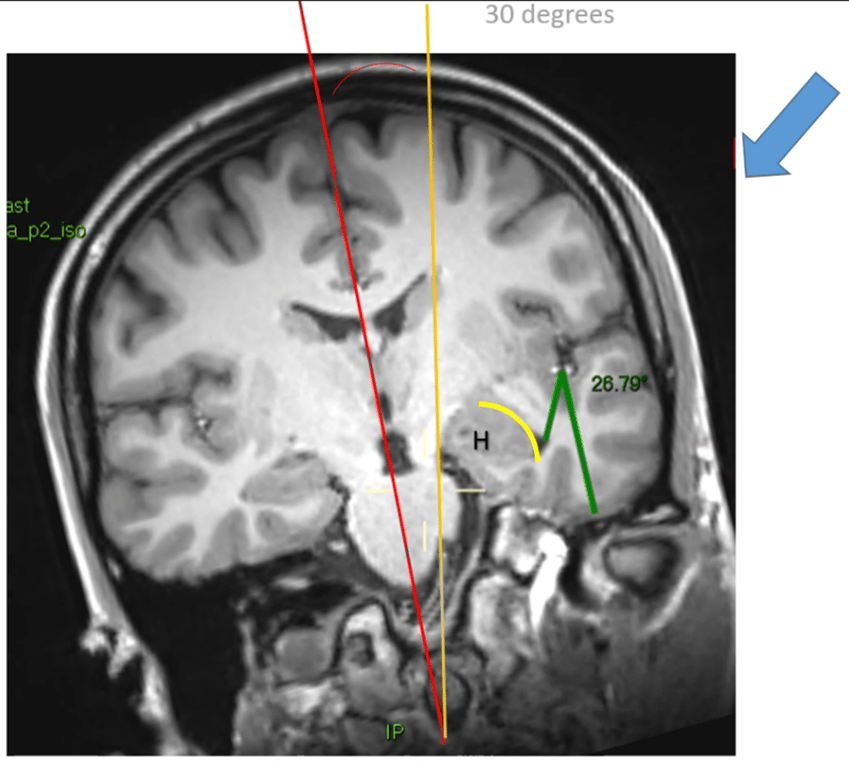
- Resections that extend more posterior
- May be associated with an increased incidence of visual field deficits, ranging from contralateral superior quadrantanopia to hemianopsia due to disruption of Meyer’s loop of visual fibers in the periventricular white matter surrounding the temporal horn of the lateral ventricle.
- More extensive resection of mesial temporal structures
- Including the amygdala and hippocampus has improved seizure control but injury to the anterior choroidal and posterior cerebral artery branches risks contralateral hemiparesis.
- More lateral temporal resection
- Is carried out with the intention of maximising disruption of the circuit of the epileptogenic zone while sparing the superior temporal gyrus (and limiting middle temporal gyrus resection more on the dominant side) to minimising interference with language function in the dominant hemisphere.
- Sparing of the lateral temporal neocortex in cases of epilepsy due to mesial temporal sclerosis via
- Trans-sylvian amygdalohippocampectomy
- Gamma Knife Radiosurgery targeting of mesial temporal lobe structures
Positioning of patient
- Supine
- Head turn (AG)
- 30° rotation and 15° extension of head
Approach
- Pterional craniotomy
- Orbital roof flattened
- Both lesser and greater wings of the sphenoid is drill down to the superior orbital fissure
- Dural opening where the arachnoid over the sylvian fissure is open
Approach & Surface | Advantages | Disadvantages |
Superior surface: transsylvian-transinsular approach | - Preserves the lateral and basal temporal cortex involved in language and higher cortical function. - Corticotomy along anterior part of the inferior insular sutures can be enlarged by opening forward along the area of the limen insulae. - May be combined with the transsylvian transcortical approach. | - Small working window, which may make it difficult to complete an en bloc resection of hippocampus and adjacent structures. - Entrance into temporal horn through its roof can cause Meyer’s loop injury. - Opening posteriorly along inferior insular sulcus may damage optic radiations. |
Lateral surface: transsulcal or transgyral approaches | - Technically less complex. - Directed through surface facing cranial opening. - Good window for en bloc resection of hippocampus and adjacent structures. - Good angle for approaching the posterior segment of the mesial temporal lobe. | - Produces lesion of the lateral temporal cortex (significant in the dominant hemisphere). - May cause injury to optic radiations if entrance into temporal horn is extended posteriorly through its lateral wall. - Significant distance between the lateral surface of temporal lobe and temporal horn. |
Basal surface: transsulcal or transgyral approaches | - Preserves the lateral temporal cortex and Meyer’s loop, because entrance into temporal horn is through its floor. - May allow access to the posterior segment of the mesial temporal lobe, depending on the position of the vein of Labbé. - Shorter route through brain to temporal horn than the lateral approaches. | - Required cerebral retraction may damage basal temporal cortex. - Risks damage to vein of Labbé. - Language dysfunction may result from cortical incision or retraction of dominant fusiform gyrus. |
Medial surface (anterior approach): transsylvian transcortical approach | - Preserves lateral and basal temporal cortices. - Preserves Meyer’s loop, because entrance into temporal horn is through its medial wall. - Proximal control of internal carotid, posterior communicating artery, anterior choroidal, and posterior cerebral arteries. - Allows recognition of medial surface anatomy before entrance into temporal horn. - May be combined with transsylvian-transinsular approach. | - Entrance into temporal horn through basal cisterns is technically more demanding because of deep, narrow window. - Limited access to posterior part of medial temporal region. - Requires posterior retraction of temporal pole and apex of uncus. - Risk to structures in basal cisterns, especially oculomotor nerve. |
Medial surface (posterior approaches): occipital interhemispheric and supracerebellar transtentorial approaches | - Preserves lateral and basal temporal cortices. - Preserves optic radiations because entrance into temporal horn is through its medial wall and floor. - Avoids retraction of temporal lobe. | - Requires occipital lobe or cerebellar retraction. - Hemorrhage with cutting through the tentorium. - Difficult access to middle segment of mesial temporal region and access to all the anterior segment is not possible. - Lack of proximal control of posterior cerebral and anterior choroidal arteries. - Early exposure of venous drainage of arteriovenous malformation. - Greater working distance. |
Standard sub-pial anterior temporal lobectomy 3 stages
Neocortical removal
- Exposing the temporal lobe
- Cortical resection is performed
- Sparing superior temporal gyrus OR
- Including the superior temporal gyrus
- Size of corticotomy
- 3–6 cm of anterior temporal neocortex is resected (depending on hemispheric language dominance), permitting access to resection of mesial structures.
- Modification
- Limited neocortical resection (3.5 cm from the temporal pole) + spares the superior temporal gyrus
- Obviating the need for language mapping in most cases
- Blind resection through the white matter of the temporal lobe can injure lead surgeon to accidentally damage the
- Optic tract
- Basal ganglia
- Meyer's loop
- Useful landmark
- Tentorial edge
- As long as the surgeon aims his neocortical temporal resection lateral to the free edge of the tentorium, there will not be any risk of entering the sylvian fissure or the inferior circular sulcus of insula or violating any diencephalic or mesencephalic structure; frequently, at this stage, the temporal horn is entered through its roof.
- Stayed below imaginary line from the inferior choroidal point and the M1 trifurcation. (Mr Grivas)
- So not to enter the basal ganglia
- Stay lateral and inferior to the optic tract
- So not to enter the thalamus and basal ganglia
- Once the temporal horn has been entered, the hippocampus and the collateral eminence are identified
- The neocortical removal can be limited medially by the collateral eminence, which indirectly indicates the superolateral limit of the collateral sulcus on the basal surface of the temporal lobe
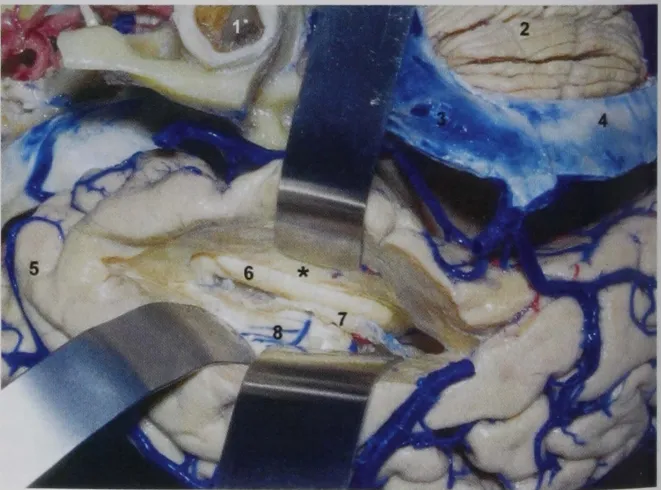
Image
- Right temporal lobe exposure for standard anatomic temporal lobectomy and amygdalohippocampectomy
- 1, Inferior temporal gyrus;
- 2, Middle temporal gyrus;
- 3, Superior temporal gyrus;
- 4, Superficial Sylvain vein.
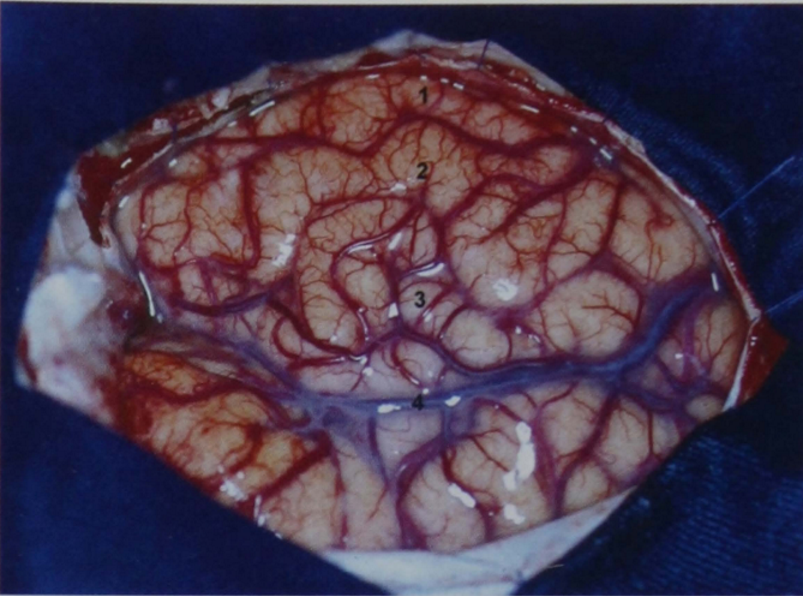
- Neocortical removal.
- The removal of the neocortex is performed either sparing or including the superior temporal gyrus.
- Keep the neocortical temporal resection laterally to the tentorial edge, there will be no risk of entering the sylvian fissure or injuring any diencephalic or mesencephalic structure.
- The anteroposterior extent of the neocortical removal varies from author to author;
- Ranges from 4.5 to 5.0 cm on the nondominant hemisphere and 3.5 to 4.0 cm on the dominant hemisphere.
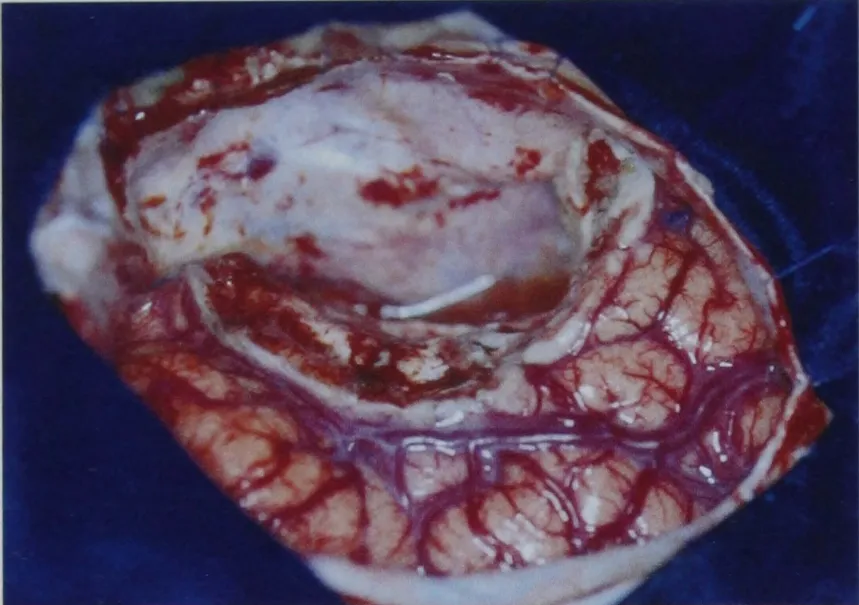
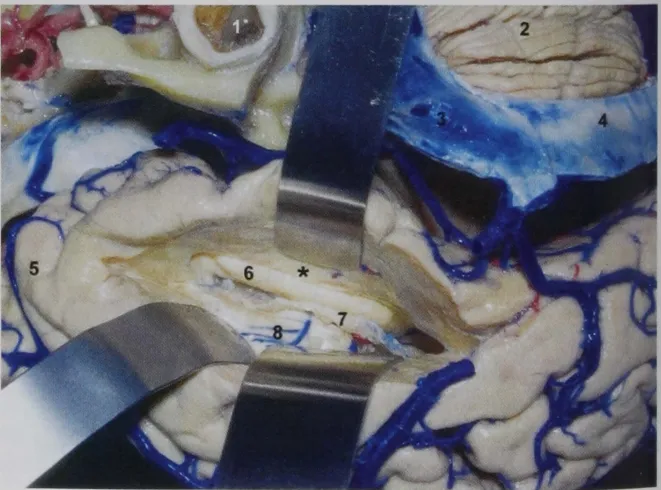
- Surgical view of the right temporal lobe after the neocortical removal.
- Frequently, during the neocortical removal, the temporal horn is entered; in this picture, the choroid plexus has been retracted medially (under the spatula), and the body of the hippocampus has been retracted laterally by a dissector.
- 1, Dura mater of the middle fossa;
- 2, Arcuate eminence;
- 3, Collateral eminence;
- 4, Head of the hippocampus;
- 5, Fimbria;
- 6, Inferior choroidal point;
- 7, Spatula;
- 8, Superficial sylvian vein.
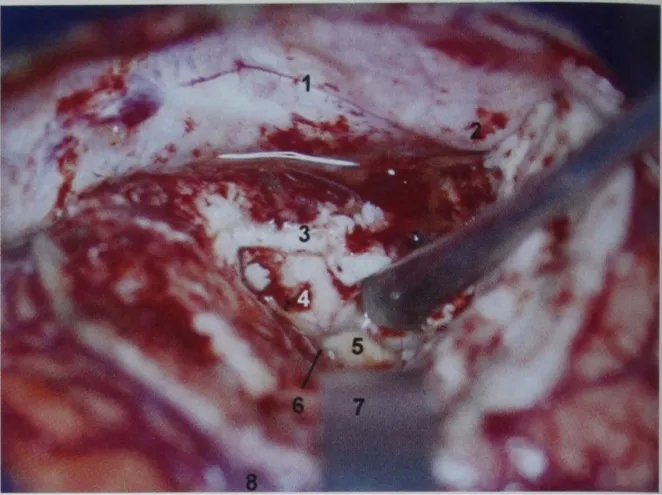
- Frequently, during the neocortical removal, the temporal horn is entered; after entering the temporal horn, the intraventricular structures are identified.
- The neocortical removal can be limited medially by the collateral eminence, which indicates the superolateral limit of the collateral sulcus.
- 1, External acoustic meatus;
- 2, Cerebellum;
- 3, Sigmoid sinus;
- 4, Transverse sinus;
- 5 , Temporal pole;
- 6, Hippocampus;
- 7, Choroid plexus;
- 8, Roof of the temporal horn;
- *, Collateral eminence.
Hippocampectomy: based on 4 anatomical steps
Opening of the choroidal fissure
- The choroidal fissure can be opened by splitting the taenia fimbriae,
- A layer of ependymal covering that attaches the choroid plexus to the fimbria, leaving the choroid plexus attached to the thalamus
- How to find the choroidal fissure
- Inside the temporal horn follow the choroid plexus
- Importance of choroidal fissure
- All structures located laterally to the choroidal fissure can be removed, and all of the structures located medially to it should be preserved.
- Choroidal fissure starts at the inferior choroidal point
- Anterior portion of the opened choroidal fissure
- Structures visible
- Arachnoidal membrane, which covers the ambient cistern
- Posterior cerebral artery and its branches
- Basal vein can be identified.
- Posterior portion of the choroidal fissure:
- Structures visible
- Parahippocampal gyrus
- Pulvinar of the thalamus
Anterior disconnection ("freeing" the head of the hippocampus)
- Consists of "freeing" the head of the hippocampus by disconnecting it from the
- Uncal recess anteriorly and inferiorly
- Medial wall of the temporal horn;
- The medial wall of the temporal horn anterior to the inferior choroidal point is the head of the hippocampus itself.
- The uncal recess and the head of the hippocampus are followed medially up to the medial wall of the temporal horn interior to the inferior choroidal point.
- The uncal recess and the head of the hippocampus will lead us toward the apex and the posterior segment of the uncus, respectively.
- The removal of the medial wall of the anterior aspect of the temporal horn by following the uncal recess and the head of the hippocampus will expose
- Arachnoid membrane medial to the apex and the posteromedial surface of the uncus and the structure within
- Oculomotor nerve
- P2A segment of PCA encircling the crus cerebri
- It is important to emphasize that the visualization of the oculomotor nerve and the posterior cerebral artery means that the inferior portions of the apex and the posteromedial surface of the uncus have been removed, but not the superior portions of them; as stated above, in the great majority of cases, the P2A segment of the posterior cerebral artery is related to the inferior portion of the posteromedial surface of the uncus; therefore, there is still the superior portion to be removed.
- After "freeing" the anterior portion of the anterior temporal horn, the anterior disconnection is continued laterally up to the collateral eminence. The anterior disconnection proceeds medially and posteriorly until the choroidal fissure is reached;
Medial disconnection
- Consists of separating the mesial temporal structures from the contents of the crural and the ambient cisterns through the already opened choroidal fissure.
- This separation is based on the identification of the arachnoid membrane that covers the contents of the ambient cistern and on the division of the hippocampal arteries.
- After the opening of the choroidal fissure through the taenia fimbriae, there is an additional arachnoid membrane with vessels entering the temporal lobe below the head of the hippocampus and perpendicular to that of the ambient cistern, usually before reaching the arachnoidal membrane of the ambient cistern.
- This is the arachnoid membrane carrying the hippocampal arteries and veins through the hippocampal notch, and these vessels should be disconnected to free the head of the hippocampus.
- This arachnoid membrane separates the inferior surface of the posterior segment of the uncus superiorly from the parahippocampal gyrus inferiorly.
- Now the rest of the hippocampus can be freed through the choroidal fissure and can be connected to the "free" head of the hippocampus.
- However, soon after splitting the taenia fimbria (the lateral posterior choroidal and anterior choroidal arteries and the inferior ventricular vein are kept intact on the thalamic side, because the choroid plexus is maintained intact and attached to the thalamus), the arachnoid membrane of the ambient cistern comes into view;
- Again, there is another arachnoid membrane that is perpendicular to that of the ambient cistern and is directed toward the temporal lobe a short distance below the fimbria, and once again, this arachnoid membrane carries the hippocampal arteries and veins through the hippocampal sulcus.
- These vessels should be disconnected to free the body and the tail of the hippocampus.
- This part of the hippocampal sulcus, located behind the head of the hippocampus, is another important landmark as it separates the dentate gyrus superiorly from the parahippocampal gyrus inferiorly
Posterior disconnection
- Directed from the choroidal fissure laterally toward the floor of the middle fossa or toward the tentorium, depending on the extent of the hippocampus to be removed.
- If the whole hippocampus should be removed, the landmark that denotes the end of the tail of the hippocampus is where the tail of the hippocampus meets the calcar avis, the inferior prominence on the medial wall of the atrium of the lateral ventricle (Figs. 73 and 74).
- After the removal of the lateral and medial temporal cortex along with the mesial temporal structures that include the hippocampus, fornix, and parahippocampal gyrus, the neural and vascular elements of the ambient cistern come into view:
- Crus cerebri,
- Tegmentum of the midbrain,
- Posterior cerebral artery
- Basal vein of Rosenthal
- Trochlear nerve
- Superior cerebellar artery
- The lateral disconnection has already been performed by the time of the neocortical removal.
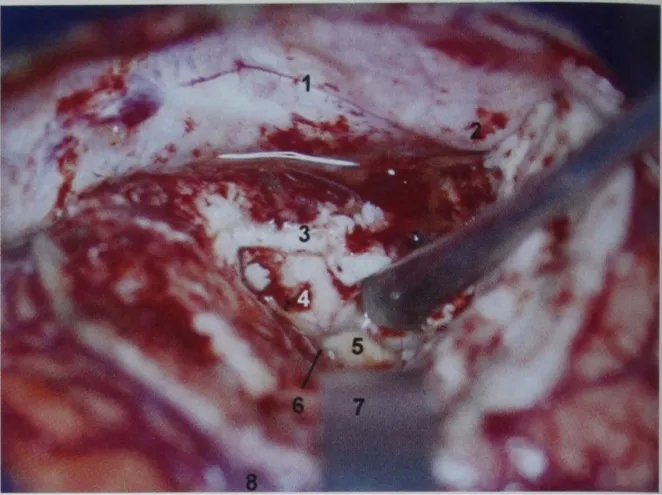
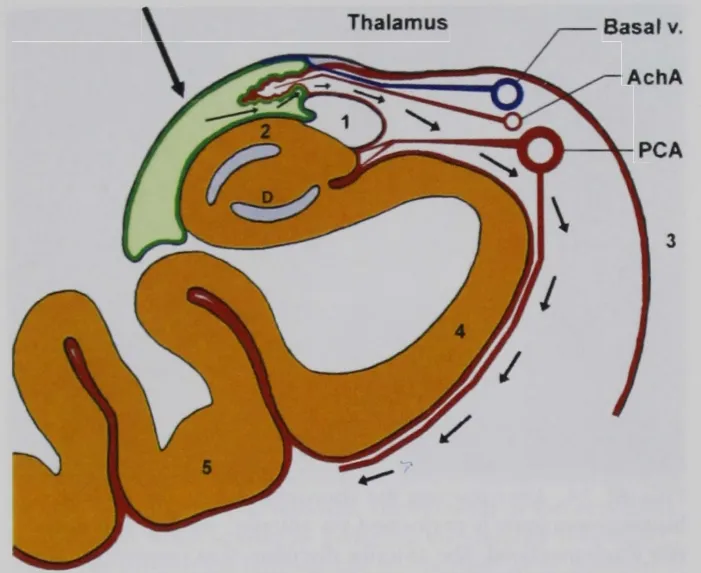
Images
- The dotted line displays the lines of disconnection, a and b, anterior disconnection; c, posterior disconnection.
- The medial disconnection is performed via the choroidal fissure
- 1, Middle fossa dura mater;
- 2, Body of the hippocampus;
- 3, Head of the hippocampus;
- 4, Fimbria;
- 5, Tail of the hippocampus;
- 6, Inferior choroidal point.

- The arrows indicate the route for medial disconnection.
- 1, Fimbria;
- 2, Hippocampus;
- 3, Brainstem;
- 4, Parahippocampal gyrus;
- 5, Fusiform gyrus.
- D, Dentate gyrus.
- Surgical view of the right temporal lobe after the neocortical removal.
- Frequently, during the neocortical removal, the temporal horn is entered; in this picture, the choroid plexus has been retracted medially (under the spatula), and the body of the hippocampus has been retracted laterally by a dissector.
- 1, Dura mater of the middle fossa;
- 2, Arcuate eminence;
- 3, Collateral eminence;
- 4, Head of the hippocampus;
- 5, Fimbria;
- 6, Inferior choroidal point;
- 7, Spatula;
- 8, Superficial sylvian vein.
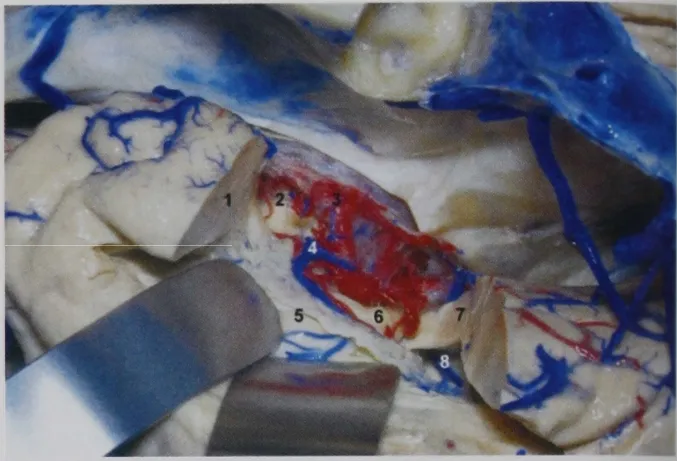
- After the removal of the lateral and basal temporal cortex along with the mesial temporal structures (hippocampus, fimbria, parahippocampal gyrus, but not amygdala), the neural and vascular elements of the ambient cistern (covered by arachnoid membrane) come into view.
- 1, Anterior disconnection;
- 2, Crus cerebri;
- 3, Posterior cerebral artery;
- 4, Basal vein;
- 5, Choroid plexus and roof of the temporal horn;
- 6, Pulvinar of the thalamus;
- 7, Parahippocampal gyrus;
- 8, Atrium.
- 1, External acoustic meatus;
- 2, Cerebellum;
- 3, Sigmoid sinus;
- 4, Transverse sinus;
- 5, Temporal pole;
- 6, Hippocampus;
- 7, Choroid plexus;
- 8, Roof of the temporal horn;
- *, Collateral eminence.
Amygdalectomy
- = removal of the uncus (Amydala is within uncus)
- In the subpial anterior temporal lobectomy, in which the uncus is approached subpially from its lateral aspect, the arteries constitute the most important anatomic landmarks for this purpose.
- Anteromedial surface of the uncus is related to the internal carotid artery and the proximal half of the Ml segment of the middle cerebral artery;
- Inferior portion of the vertex of the uncus is related to the oculomotor nerve;
- Inferior portions of the posteromedial surface of the uncus are related to the P2A segment of PCA turning around the crus cerebri
- Superior portions of the posteromedial surface of the uncus are related to the posterior part of the cisternal segment of the anterior choroidal artery just before entering the temporal horn through the choroidal fissure.
- Superiorly, there is no clear demarcation between the amygdala and the globus pallidus.
- Subpial resection of the uncus can be deemed adequate when the following vascular landmarks is visualised through the Pia:
- Anterior and anterior-medially:
- The visualisation of ICA and the proximal segment of the MCA indicates that the anteromedial surface of the uncus has been removed;
- Inferiorly:
- Visualisation of the oculomotor nerve
- Posterior medially:
- P2A segment of the posterior cerebral artery
- Superiorly:
- Optic tract: Hard to visualise
- Posterior portion of cisternal segment of the anterior choroidal artery, as it runs under the optic tract;
- Initial portion of the cisternal segment of the anterior choroidal artery does not always follow the superior portion of the uncus, whereas its posterior portion, close to the inferior choroidal point, is constantly related to the superior portion of the posteromedial surface of the uncus.
- Carotid-choroidal line:
- A line is traced from the bifurcation of the internal carotid artery or the proximal segment of Ml to the inferior choroidal point
- Almost the entire uncus will stay below this line.
- It is not advisable to cross this line superiorly because of the risk of invading the globus pallidus
- Intraventricularly, the posterior portion of the amygdala is the prominence on the roof of the temporal horn immediately anterior to the inferior choroidal point, which passes below this line, and it can be removed until this line is established,
- Posterosuperior:
- The inferior choroidal point.
- The highest point of the uncus
Visualisation
- Finally, after the complete removal of the temporal lobe, including the amygdala and the hippocampus, the surgeon must be able to visualize the following structures through the arachnoid membrane:
- The internal carotid,
- Middle cerebral,
- Posterior communicating,
- Anterior choroidal, and
- Posterior cerebral arteries,
- The oculomotor nerve,
- The basal vein,
- The crus cerebri,
- The lateral mesencephalic sulcus and vein,
- The tegmentum of the mesencephalon,
- Sometimes the fourth nerve and the superior cerebellar artery
Post op instructions
- An increased seizure frequency in the immediate post-op period is very common.
- Patients should continue to take their anti-epileptic medication for 2 years following surgery.
- Some units prescribe a short course of oral dexamethasone.
- The DVLA should be notified and driving advice followed, as per their guidance.
Outcome
- In + MRI findings pre-operatively,
- 80% will have a substantial (at least 50%) reduction in seizure frequency; 50% of cases will be seizure free at 2 years.
- In normal MRI
- 50% will have reduced seizure frequency post-op.
Complications
- Significant neuropsychological deficits
- Visual field defect in 5%, preventing driving
- Reduction in verbal, visual memory
- Possible psychiatric disturbance