Approach
Surgical anatomy and biomechanics
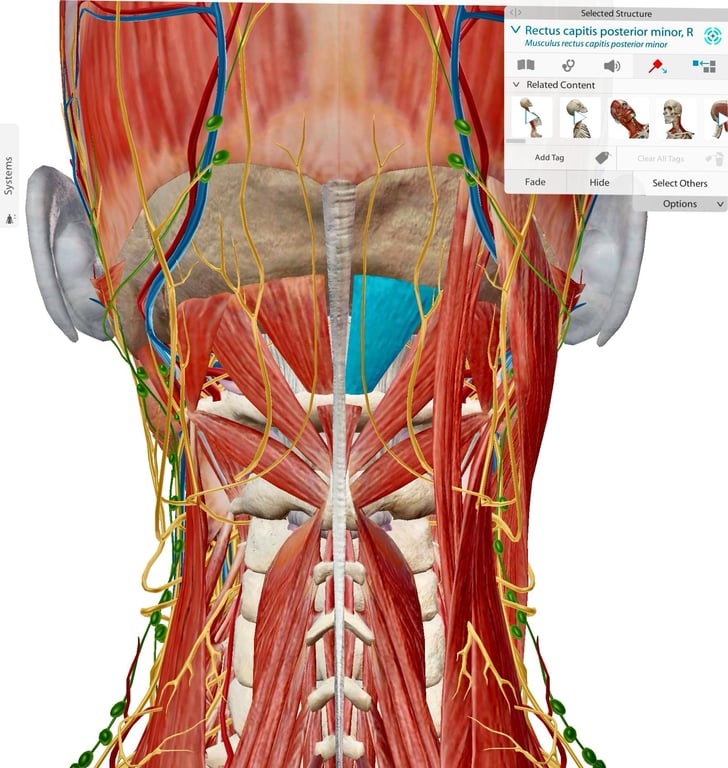
Muscle
- Rectus capitis posterior minor: the only muscle attached to C1 posteriorly
- If detached it can be swiped laterally to protect from vertebral artery
Nerves
- C1:
- Motor only nerve
- Rectus capitis muscles, omohyoid, thyrohyoid and geniohyoid.
- Suboccipital nerve Aka posterior ramus of the first cervical spinal nerve (C1)
- C2:
- Motor and sensory nerve
- Rectus capitis muscles, omohyoid, sternohyoid, sternothyroid and longus colli.
Movements
- C0/C1 about 15° of flexion and extension
- C1/ C2 articulation contributes to 45° of rotation which is about 50% of the rotation occurring by the cervical spine.
Ligaments
- Transverse ligament
- attached to a tubercle on the medial aspect of one C1 lateral mass to the other
- located posterior to the dens
- transverse ligament limits flexion and anteroposterior (AP) translation of the atlantoaxial articulation.
- Alar ligaments
- attached from dorsolateral dens passing rostro- lateral to the medial tubercle of the occipital condyle at the anterior lip of foramen magnum.
- Limits atlanto- occipital rotation.
- Supplementary ligaments
- Apical ligament
- Anterior atlanto- occipital and tectorial membranes
- In continuity with the ALL and posterior longitudinal ligament (PLL)
- Posterior atlanto- occipital membrane and ligamentum flavum.
- The longitudinal fibres dorsal to the transverse ligament complete the formation of the cruciate ligament
Alignment
- cervical lordosis (77%) is located in C0-C2
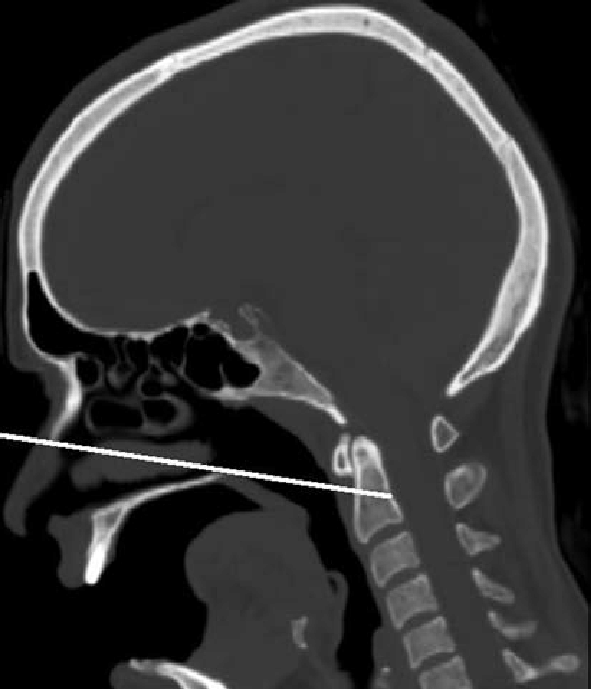
- assessed radiologically via the angle between McGregor’s line and the inferior end plate of C2
- T1 slope correlates with C0-C7 angle (angle between McGregor line and the inferior end plate of C7
- patients with increased T1 slope will require greater C0-C7 angles to mainatina horizontal gaze
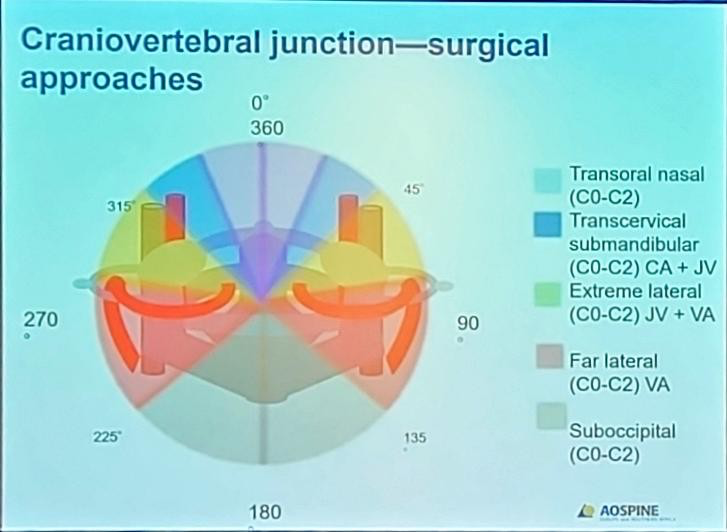
Anterior
- Anterior transoral and transnasal odontoidectomy + C1/ 2 fixation
- Indicated:
- there is a need for anterior decompression and resection of the dens.
- They are now rarely indicated for rheumatoid disease as rheumatoid pannus normally resolves following posterior fusion alone.
- For compressive Type 2 Odontoid peg fractures
- Techniques
- Approaches
- Patients are positioned supine with biplanar intraoperative fluoroscopy available.
- Neuro-navigation can also be used.
- Open OR
- Endonasal Endoscopic Extended surgical approaches
- Endoscopic odontoidectomy is considered in cases of basilar invagination.
- The nasopalatine line (as described by Kassam— which is a line on the midline sagittal images from the inferior tip of the nasal bone to the posterior aspect of the hard palate extended to the anterior spine) is used to indicate the lower limit of this approach.
- The high-riding dens found in cases of basilar invagination, allows endoscopic drilling at the base of the odontoid.
- Further inferior extension, if required, can be performed with a transoral endoscopic assisted approach.
- A direct incision in the nasopharyngeal wall in the midline or a flap is used to expose the lower clivus, anterior lower lip of the foramen magnum and anterior arch of the atlas. This approach avoids the need for a palatal incision. The anterior arch of the atlas is resected using a high- speed drill and the base of the odontoid is drilled and ‘egg- shelled’ until the underlying transverse ligament and dura are reached and disconnected from the C2 body.
- The bone is then carefully pulled down from the foramen magnum and may require additional removal of the anterior lip of this foramen to allow sharp (a) division of the apical and alar ligaments.
- The totally free odontoid bone is removed and the theca is decompressed
- The edges of the incision are approximated and do not necessarily require suturing, unless there is cerebrospinal fluid (CSF) leak.
- Subsequently fixation is required as this procedure makes C1/ 2 unstable.
- If extended exposure is required, a transoral mandibular splitting approach is used. The use of anterior techniques is largely confined to specialist centres.
- Two fixation techniques are available:
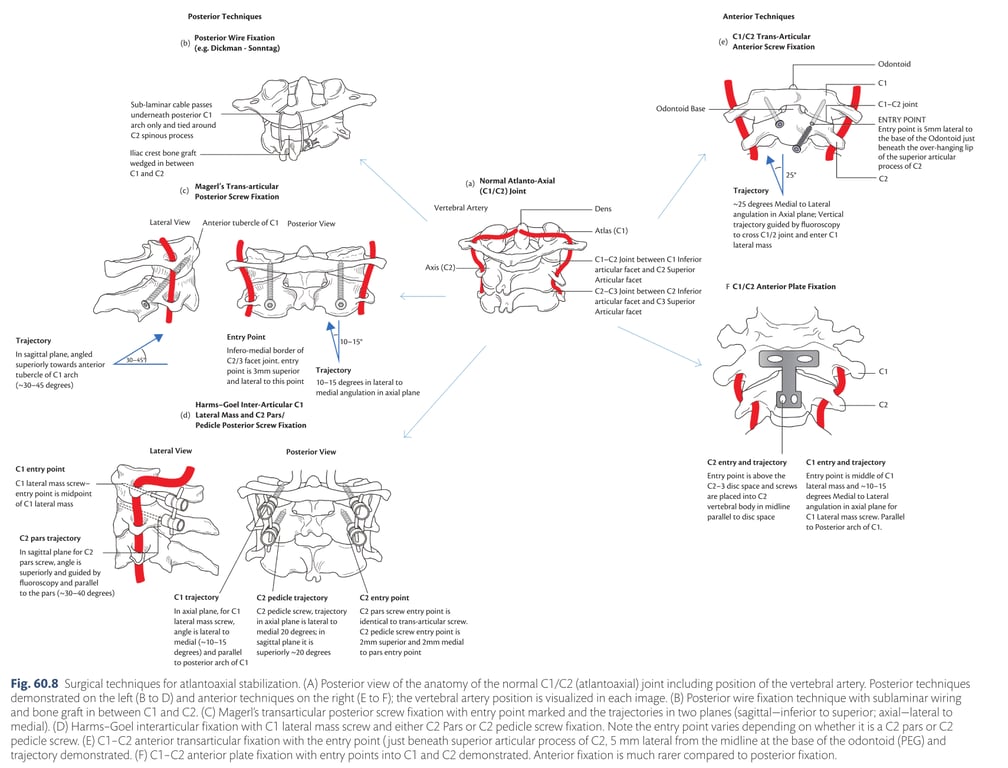
- C1- C2 transarticular screws or
- The pharyngeal mucosal incision is linear
- T- plate fixation with C1 lateral mass and C2 vertebral body screws (Fig. 60.8).
- The pharyngeal mucosal incision is T- plate a U- shaped flap
- Vertebral artery injury is avoided by keeping the lateral dissection within 12 mm of the midline at the C2 vertebral body.
- CI
- Oropharyngeal infection
- Complications
- injury to viscera including the oesophagus, trachea, pharynx, tongue, internal carotid artery, internal jugular vein, and cranial nerves IX– XII.
- Complication related to healing of the pharyngeal mucosal flap
- Velopharyngeal incompetence with regurgitation
- Speech dysfunction from soft palate incision
- if needed and teeth malocclusion due to the osteotomies for transmaxillary or transmandibular approaches.
- C1 lateral mass to C2 vertebral body plate and screw fixation
Posterior
- General
- Fixing from the occiput to C2 or the subaxial cervical spine is a morbid procedure, which patients find disabling, rendering the occipitoatlantal +/ – the atlantoaxial joints completely immobile. It should only be utilized where other methods will not suffice
- Indication
- Occipitocervical dislocation
- Grossly unstable C1 fracture where this surgical option is preferred
- Basilar invagination
- Displaced C2 peg fracture causing neurology
- Planning
- Plan preoperatively (including CT scanning +/ – contrast) with particular attention to any venous anomalies which would prevent safe screw placement.
- Positioning
- Careful intraoperative positioning to ensure as ‘anatomical’ a position as possible is vital:
- an overly flexed position can make it extremely difficult to swallow;
- an overly extended position makes it difficult to walk due to an inability to see one’s feet and an alteration of sagittal balance.
- Approach
- Incision is made from the external occipital protuberance inferiorly (the lower limit depending upon the planned lower limit of the fixation).
- Muscles are stripped to expose the occipital bone and the laminae and lateral masses.
- Techniques
- Cons
- Requires an intact posterior ring of C1 and C2 lamina.
- Needs to be used together with
- Halo after surgery in order to achieve a satisfactory fusion rate.
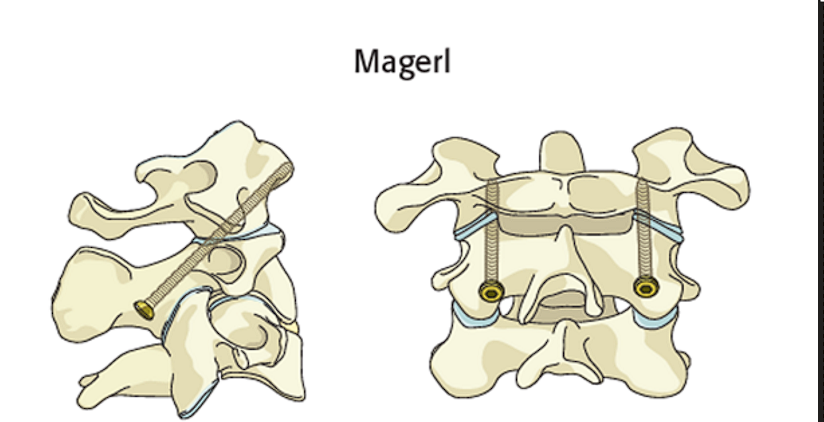
- C1–C2 transarticular screws
- Technique
- A single screw on each side is placed through the pars interarticularis of C2 passing through the C1/ 2 joint directed at the lateral mass of C1
- care must be taken to avoid anterior perforation of the C1 lateral mass, which could result in injury to the pharynx, internal carotid artery, and/ or lower cranial nerves.
- Intraoperative fluoroscopy guides the screw trajectory.
- The patient is positioned prone in a skull clamp with neck flexion.
- The C1 posterior arch and lateral masses, C2 laminae, C2 pars and the C2/ 3 facet joints are exposed.
- Separate stab incisions caudally may be required to achieve the trajectory for the transarticular screw (usually 1– 2 cm lateral to C7/ T1 spinous process).
- The C1/ 2 joint capsule can be opened to denude the articular surface.
- Drilling for screw placement is guided with fluoroscopy or alternatively intraoperative navigation can be used.
- The C1/ 2 transarticular screw is placed after tapping the hole.
- Bone graft can be sited on exposed bone surfaces to supplement the fusion.
- The fixation is often augmented by a Dickmann– Sonntag posterior sublaminar wire.
- Most stable and rigid fixation biomechanically of the C1/ 2 joint
- Almost complete obliteration of rotation.
- Contraindication
- anomalous high-riding vertebral artery.
- A preoperative CT Angiogram helps define the course of the vertebral artery.
- It is technically demanding with increased risk of vascular injury
- Cons
- Transarticular screws cannot be inserted on at least one side in 20% of cases due to the location of the vertebral artery.
- The screws are difficult to insert in obese patients because the proper screw trajectory cannot be achieved.
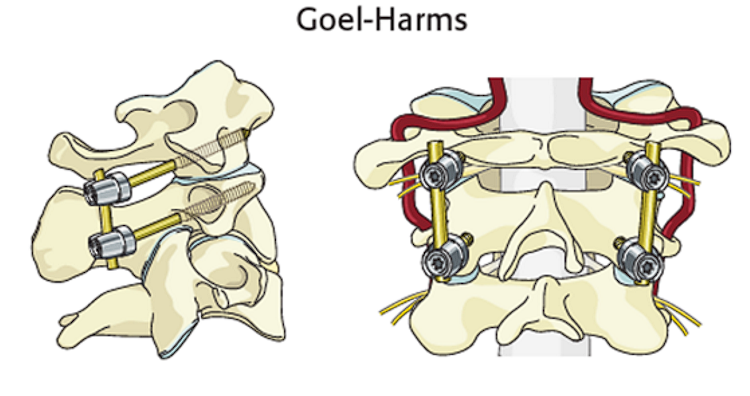
- Harms and Melcher (2001) and Goel et al. (2002) employed an interarticular fixation with C1 lateral mass and C2 pars/ pedicle screws as an alternative to C1/ 2 transarticular fixation.
- Pros
- Anatomic reduction of C1/ 2 is not essential
- It can be used with a high-riding vertebral artery.
- The positioning and exposure are as for the transarticular screw technique.
- Preservation of the C2 nerve root is optional.
- Fusion rates are high.
- Internal screw fixation is biomechanically superior to wire/ clamp techniques as it directly inhibits motion at the C1/ 2 articular surfaces.
- Technique
- Complications
- Vertebral artery injury (<5%)
- which can occur during exposure or screw placement.
- If arterial perforation occurs during screw preparation, the screw should be implanted for tamponade.
- The contralateral side is left uninstrumented and the patient should have an angiogram to assess the posterior cerebral circulation.
- If C1/ 2 screw fixation is not possible, use alternative strategies
- occipito- cervical fixation
- external orthotic stabilization with a HALO.
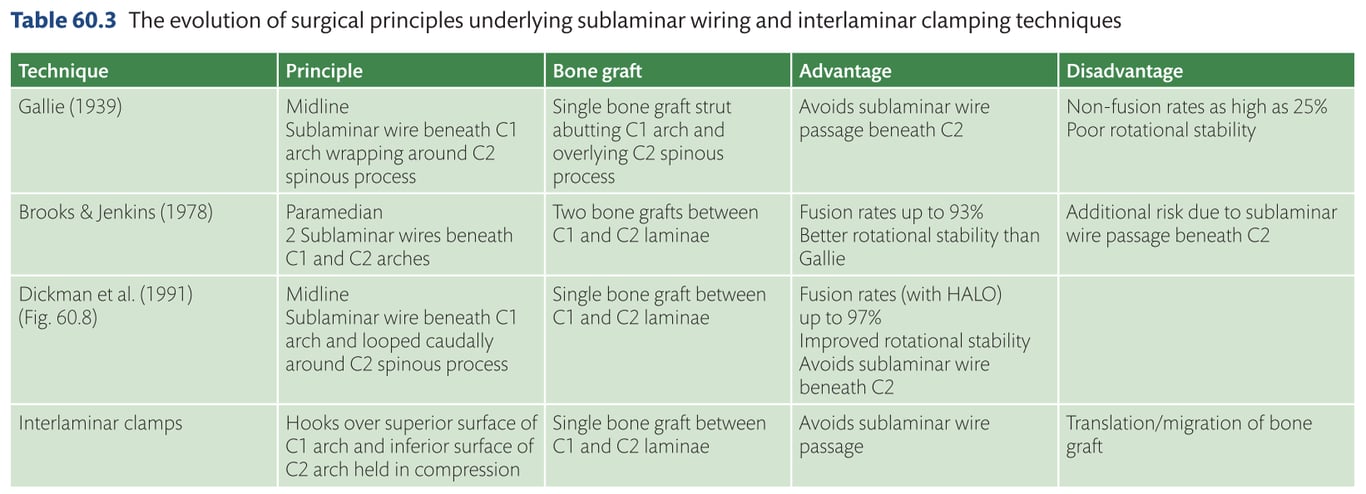
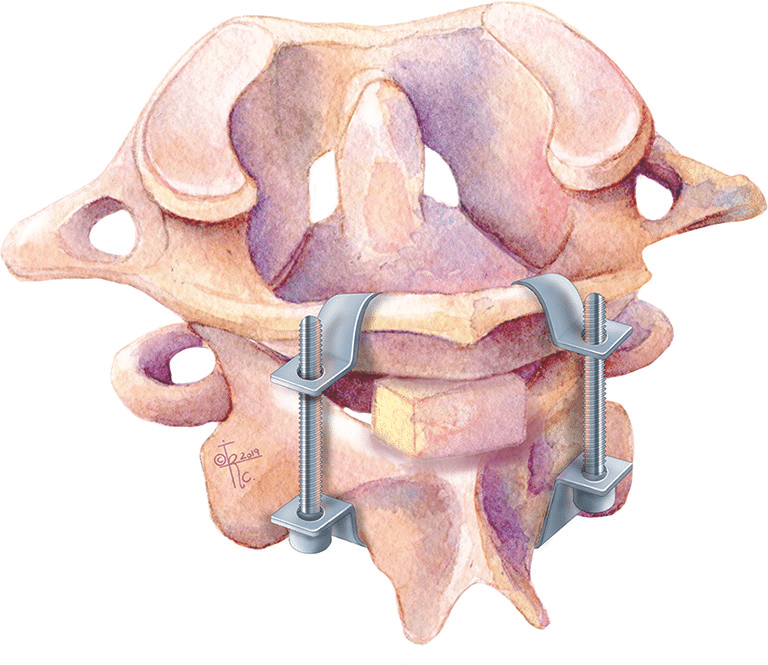
Sublaminar wiring (Gallie, Brooks- Jenkins, Dickman- Sonntag) and interlaminar clamps
Magerl’s C1/ 2 transarticular screws
Harms– Goel C1 lateral mass and C2 pars/ pedicle screws
- Techniques
- Rods
- contour a straight rod to fit
- Prebent rods exist,
- Need little further contouring
- are stronger
- Almost always necessary to trim both ends to fit.
- Rod placement, which intuitively seems simple, can often be more awkward and time- consuming than the other parts of the procedure.
- Fusion
- decorticate all available bony surfaces and pack with bone graft material and/ or synthetic bone substitutes.
- All metalwork will fail in the long run if fusion does not occur and the head presents a large mechanical lever arm relative to the cervical spine.
- It is often necessary to carry on with external immobilisation postoperatively for a number of weeks until one is confident that fusion is occurring.
- C0 fixationC1 fixationC2 fixation
- Morbidity and mortality
- Zileli 2022 N=128
- 4.6% Early postoperative (1st month) deaths.
- Complications in 52%
- Implant-related (32%),
- Wound problems (23.4%),
- Systemic and other complications (11.7%),
- Neurologic complications (6.2%)
- Implants are removed in 24% for different reasons:
- deep wound infection (7),
- local pain and restriction of head movements (21),
- respiratory distress and swallowing problems (2),
- screw fracture and local pain (1).