General
- Technically not a true malformation and rather is more of deformation
AKA
- Primary cerebellar ectopia
- Adult Chiari 1 malformation
- Since it tends to be diagnosed in the 2nd or 3rd decade of life
Classically described as
- A rare abnormality
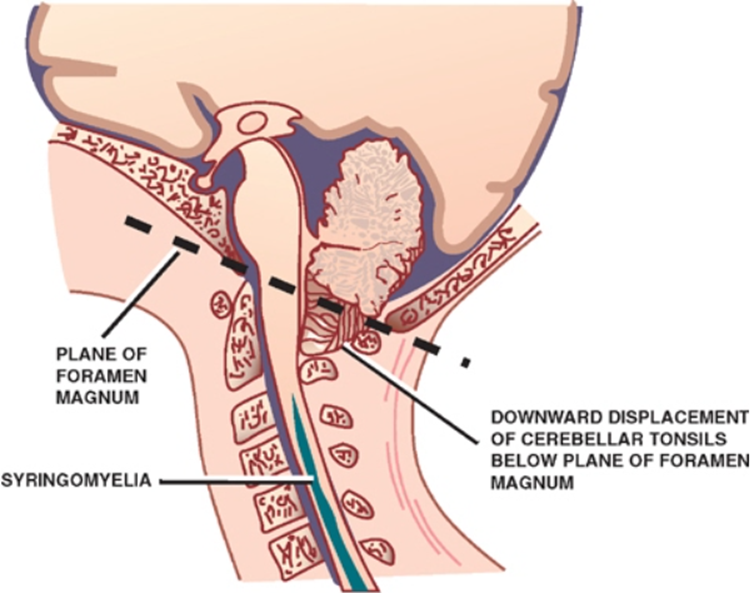
- Restricted to caudal displacement of cerebellum with tonsillar herniation below the foramen magnum (below for criteria) and
- “peg-like elongation of tonsils”
Definition
- A functional obstruction at the foramen magnum by cerebellar tonsils
- One that may result in neuraxis compression and/or obstruction to CSF flow across the craniovertebral junction’
- Should not use measurements: decent of the cerebellar tonsils > 5 mm below the foramen magnum
- Although definitions range from 0 mm (tonsils at the level of the foramen magnum) to 1.5 cm.
- Defining Chiari 1 by measurement is not only arbitrary but potentially misleading, risking both over-diagnosis and under-diagnosis
- Cerebellar tonsil descent below FM with impaction, while common, is no longer a sine qua non of diagnosis.
Aetiology
Congenital
- A small posterior fossa
- Underdevelopment of the occipital bone due to a defect in the occipital somites originating from the para-axial mesoderm
- Low lying tentorium (the roof of the p-fossa)
- Thickened or elevated occipital bone (the floor of the p-fossa)
- Space occupying lesion in p-fossa
- Arachnoid cyst (Retrocerebellar or Supracerebellar),
- Tumor (e.g. FM meningioma or cerebellar astrocytoma),
- Hypervascular dura
- Arachnoid web or scar or fibrosis around brainstem and tonsils near FM.
- Abnormalities of the upper cervical spine
- Hypermobility of the craniovertebral junction
- Klippel-Feil syndrome
- Occipitalization of the atlas
- Anterior indentation at foramen magnum: e.g. basilar invagination or retroversion of the odontoid process
- Ehlers-Danlos syndrome
- Craniosynostosis: especially cases involving all sutures
- Retained rhomboid roof: rare
Acquired
- Has been described with just about anything that takes up intracranial space
- Chronic subdural hematomas
- Hydrocephalus
- Following LP shunt (p.435) or multiple (traumatic) LPs:
- Acquired Chiari 1 malformation (may be asymptomatic)
Primary | Secondary |
Tonsilar ectopy | Cranio-spinal pressure dissociation |
Small posterior fossa | IIH, Hydrocephalus, Tumour |
Isolated abnormality | Spontaneous leak, iatrogenic leak (dural tear, LP shunt overdrainage), CSF-venous fistula |
ㅤ | CCJ anomalies (retroflexed odontoid, basilar invagination) |
Numbers
- Average age at presentation is 41 years (range: 12–73 yrs).
- Slight female preponderance (female: male= 1.3:1).
- Incidence 1:1000
- Average duration of symptoms
- If symptoms clearly related to Chiari malformation is 3.1 yrs (range: 1 month-20 yrs)
- If nonspecific complaints
- e.g. H/A, are included, this becomes 7.3 years
- This latency is probably lower in the MRI era.
Pathophysiology of Chiari I malformation
Overt hydrocephalus with ventriculomegaly
- Affects 10% of paediatric patients with Chiari 1
- Patient should undergo ICP study first
- Management
- The hydrocephalus should be treated first
- Improvement in tonsillar herniation, or indeed complete reversal of the Chiari 1 following hydrocephalus treatment, whether by VPS or ETV, is well documented
Disorder of the craniovertebral junction
- Affects 4-20% of Chiari 1 pts
- Abnormal biomechanics and anatomy of the craniovertebral junction (CVJ) rather than posterior fossa volume is the cause
- Bony malformation commonly found in Chiari 1
- Atlanto-occipital assimilation
- Basilar invagination
- Craniocervical instability
- Odontoid retroflexion
- Incidence of paediatric Chiari 1 = 80%
- Bollo et al. identified radiological parameters that increased the likelihood of occipito-cervical fixation being required.
- Descent of the obex as well as the tonsils, below the plane of the foramen magnum (Chiari 1.5),
- Basilar invagination
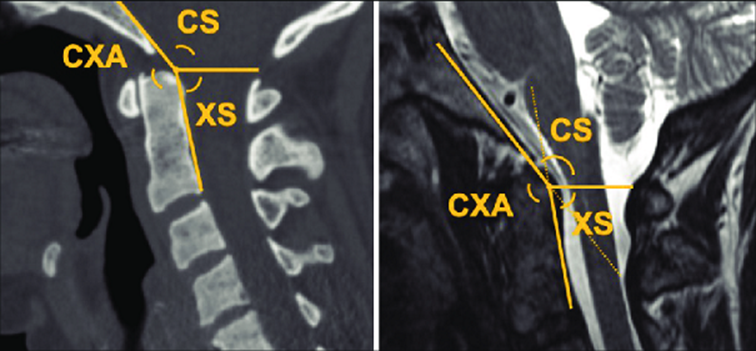
- A clivo-axial angle < 125 degrees
- Angle determined from the intersection of a line along the slope of the clivus (Wackenheims line) and a line drawn from the posteroinferior point of the C2 vertebral body up along the odontoid (posterior spinal line).
- Management
- Posterior craniocervical fixation and decompression
- Mainstay of treatment
- Is anterior decompression required
- If the CVJ abnormality is not reduceable then go for trans-oral decompression
- Ventral decompression is not without risk and does not obviate the need for a posterior procedure (fixation with or without decompression).
- The degree of odontoid retroflexion and its effect on the neuraxis are most commonly expressed by the Grabb measurement or pBC2 line.
- Grabb Oakes Measurement
- Midline MRI T2 image used
- Line drawn from Basion to the inferior(bottom), posterior aspect of the C2 bone.
- Perpendicular line drawn to the dura
- Yellow line is the Grab oakes measurement
- A normal Grabb Oakes Measurement is 9mm or less
- Ventral decompression was not required if this measure was < 9 mm.
- Increasingly, it is recognised that traction (prior to or during surgery) will adequately address ventral compression in the majority of cases, obviating the need for trans-oral surgery
Disorder of intracranial venous drainage and craniosynostosis
- Reduction of intracranial venous drainage rather than posterior fossa volume is the cause
- Interaction between venous hypertension, intracranial pressure and cerebrospinal fluid circulation is complex; disturbances in each of these have been correlated with Chiari 1
- Reversibility of the Chiari 1 was only observed when adequate venous drainage from the posterior fossa was established after therapeutic embolization
- Reduced jugular venous drainage was among the strongest predictors of poor outcome
- Reduce Jugular venous drainage → exacerbation by bulbar palsy causing chronic CO2 retention → progressive extrusion of hind brain
- Post fossa volume by itself is a bad predictor for Chiari 1 outcome
- Studies have failed to show a consistent correlation between posterior fossa volume and Chiari 1 in syndromic craniosynostosis, indicating that other mechanisms need to be explored
- Possibly post fossa venous drainage deficit is a better answer
- Jugular foraminal stenosis and collateral venous drainage are much more common among cases of syndromic craniosynostosis compared with controls
- 18/23 patients with craniosynostosis had either complete or more than 50% occlusion of one or both sigmoid/jugular sinuses
- Syndromic craniosynostosis
- Chiari 1 is present in
- Kleeblatschadel (cloverleaf skull): 100%
- Crouzon syndrome (70%)
- Pfeiffer syndrome (50%)
- Unusual in Apert syndrome (< 2%).
- Unusual in Apert because the sutures were seen to persist for longer permitting adequate growth to accommodate the maturing cerebellum
Disorder of growth and metabolism
- The Chiari I malformation is commonly a disorder of mesenchyme rather than neural tissue
- More a disorder of the ‘container than the contents’
- Growth hormone deficiency
- In one MRI study of patients with GHD, 20% of cases were found to have Chiari 1
- Basiocciput tended to be shorter, and the foramen magnum longer in cases of GHD, factors that might predispose to Chiari 1
- GHD and Chiari 1 is further strengthened by observations of improvement, not only in Chiari 1 but also syringomyelia, when GHD patients are treated with growth hormone
- Calcium and phosphate metabolism
- Due to
- Rickets due to
- Vitamin D deficiency
- Hypophosphataemic rickets: due to excessive urinary loss of phosphate
- Rickets can affect skull growth
- Chiari 1 was identified in 44% of cases of familial hypophosphataemia
- It remains to be seen whether medical management of the underlying disease can modify the natural history of the Chiari 1.
- Should Chiari 1 patient be screened for Vit D, Ca and PO4 deficiency
- Radiation
- Annual growth rate of the clivus was reduced after radiotherapy
- Metabolic bone diseases
- Eg
- Pagets disease, fibrous dysplasia, Gorehams disease and osteopetrosis
- Although it is often unclear whether the effect is mediated simply through reduced growth, or whether factors such as venous hypertension and secondary craniosynostosis, which commonly coexist these conditions, may also have a role.
Unproven and probably wrong causes of Chiari 1
- Occult tethered cord syndrome (OTCS)
- Definition: refers to a scenario in which there are clinical features compatible with a tethered spinal cord (sphincter dysfunction, low back pain, lower limb symptoms) yet on MRI, the conus is in a normal position and there are no overt features of spinal dysraphism.
- It is still not clear if OTCS is associated with Chiari 1
- How can the filum (usually less than 2 mm diameter), in the context of a normally positioned conus, to exert tension sufficient to cause traction of the brainstem
- The spinal cord is, after all, not simply anchored by the filum alone but is attached to the spinal canal along its length via the nerve roots and dentate ligaments; therefore, any (likely small) tractional forces emanating from the filum will be exerted over a limited number of segments of the lower spinal cord.
- Furthermore, in situations where the spinal cord is unquestionably low lying (for example lumbosacral lipomas), the hindbrain and cerebellum are typically normally positioned.
- Hypermobility
- Hypermobility states, in particular hereditary disorders of connective tissue (notably Ehlers-Danlos syndrome, EDS)
- Postural orthostatic tachycardia syndrome (POTS)
Clinical features
Asymptomatic
- 15–30% of patients with adult Chiari malformation are asymptomatic
Pathomechanism of clinical features
- Compression of brainstem at the level of the foramen magnum
- Hydrocephalus
- Hydrocephalus occurs in 7–9% of patients with Chiari type 1 malformation and syringomyelia.
- Syringomyelia
- Syringomyelia of the spinal cord is present in 30–70% of cases.
- True hydromyelia probably doesn’t occur;
- CSF flow has not been documented in humans, and it is generally not possible to find communication between the syrinx and the central canal in Chiari 1 patients.
- Isolation of the intracranial pressure compartment from the spinal compartment causing transient elevations of ICP intracranial pressure
Symptoms
- Pain/Headache (69%)
- Especially headache, which is usually felt in the suboccipital region
- Worsen by neck extension or Valsalva manoeuvre.
- Pain classically should not be present between coughs
- Weakness
- Is also prominent, especially unilateral grasp.
- Lhermitte’s sign
- Lower extremity involvement usually consists of bilateral spasticity.
Presenting in 71 cases
Symptom | % |
Pain | 69 |
H/A (headache) | 34 |
Neck (suboccipital, cervical) | 13 |
Girdle | 11 |
Arm | 8 |
Leg | 3 |
Weakness (1 or more limbs) | 56 |
Numbness (1 or more limbs) | 52 |
Loss of temperature sensation | 40 |
Painless burns | 15 |
Unsteadiness | 40 |
Diplopia | 13 |
Dysphasia | 8 |
Tinnitus | 7 |
Vomiting | 5 |
Dysarthria | 4 |
Dizziness | 3 |
Deafness | 3 |
Fainting | 3 |
Facial numbness | 3 |
Hiccough | 1 |
Facial hyperhidrosis | 1 |
Signs
- Classically
- Downbeat nystagmus on vertical movement
- Rotatory nystagmus on horizontal movement
- Also includes oscillopsia
- 10% will have a normal neurologic exam with occipital H/A as their only complaint.
- Some patients may present primarily with spasticity.
- Three main patterns of clustering of signs
- Foramen magnum compression syndrome (22%)
- Ataxia
- Corticospinal and sensory deficits
- Cerebellar signs
- Lower cranial nerve palsies
- Severe H/A (37%)
- Central cord syndrome (65%)
- Dissociated sensory loss
- Loss of pain & temperature sensation with preserved touch & JPS
- Occasional segmental weakness
- Long tract signs (syringomyelic syndrome)
- Lower cranial nerve palsies (11%)
- Cerebellar syndrome (11%)
- Truncal and limb ataxia
- Nystagmus
- Dysarthria
Presenting in 127 patients
Sign | % |
Hyperactive lower extremity reflexes | 52 |
Nystagmus | 47 |
Gait disturbance | 43 |
Hand atrophy | 35 |
Upper extremity weakness | 33 |
“Cape” sensory loss | 31 |
Cerebellar signs | 27 |
Hyperactive upper extremity reflexes | 26 |
Lower cranial nerve dysfunction | 26 |
Babinski sign | 24 |
Lower extremity weakness | 17 |
Dysesthesia | 17 |
Fasciculation | 11 |
Horner sign | 6 |
Natural history
- The natural history is not known with certainty (only 2 reports on “natural history” exist).
- A patient may remain stable for years, with intermittent periods of deterioration.
- 50% remain stable for long periods
- Rarely, spontaneous improvement may occur (debated).
- Spontaneous resolution is rare
- Progression to quadriplegia is rare
- ? Some deterioration inevitable
- Occasional sudden deterioration
Evaluation
Ophthalmology assessment for papilledema
Skull XR
- Only 36% were abnormal
- 26% showed basilar impression
- 7% platybasia
- 1 patient each with Paget’s and concave clivus
- In 60 C-spine X-rays, 35% were abnormal
- Assimilation of atlas
- Widened canal
- Cervical fusions
- Agenesis of posterior arch of atlas
Unenhanced CT
- CT is poor for evaluating the foramen magnum region due to bony artifact.
- It is very good at demonstrating hydrocephalus (as is MRI).
- When combined with intrathecal iodinated contrast (myelogram), reliability improves.
- Findings
- Tonsillar descent with possible complete blockage of dye at foramen magnum.
MRI of brain and C-spine
- Diagnostic test of choice
- Findings
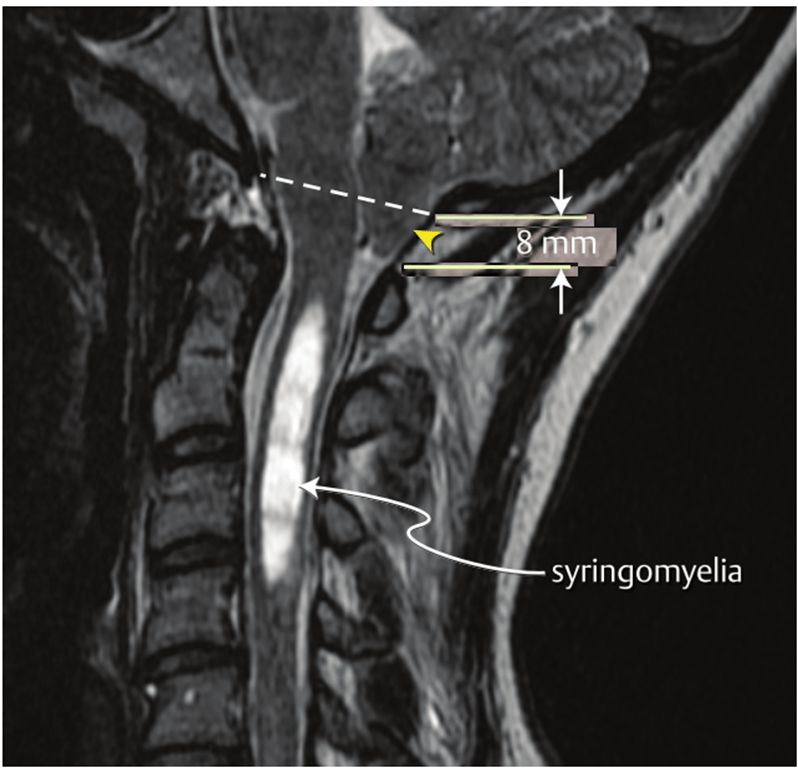
- Location of cerebellar tonsils below foramen magnum
- ᵃBased on measurements in 200 normals and 25 Chiari I patients taken in relation to the lower part of the foramen magnum
- Criteria for Chiari I
- > 5mm was defined as clearly pathologic (with 3–5mm being borderline)
- Conversely, 14% of patients with tonsillar herniation > 5mm are asymptomatic (average extent of ectopia in this group was 11.4 ± 4.86 mm).
- Tonsillar position relative to FM at various ages
- ᵃnegative number indicates distance below FM
- ᵇS.D. = standard deviation. Descent > 2 S.D. beyond normal is suggested as a criteria for tonsillar ectopia
- Potentially more significant than the absolute tonsillar descent is the amount of compression of the brainstem at the FM, best appreciated on axial T2WI MRI through the FM.
- Complete obliteration of CSF signal and compression of the brainstem at the FM by impacted tonsils is a common significant finding.
- Ventral brainstem compression when present.
- Other
- Hydrocephalus
- Empty sella
Tonsillar herniation
Group | Meanᵃ | Range |
Normal | 1 mm above | 8 mm above to 5 mm below |
Chiari I | 13 mm below | 3–29 mm below |
Criteria for lowest extent of tonsils accepted as normal | Sensitivity for Chiari I | Specificity for Chiari I |
2 mm below FM | 100% | 98.5% |
3 mm below FM | 96% | 99.5% |
Age (years) | Normal (mm)ᵃ | 2 S.D.ᵇ(mm) |
0–9 | –1.5 | –6 |
10–19 | –0.4 | –5 |
20–29 | –1.1 | –5 |
30–39 | 0.0 | –4 |
40–49 | 0.1 | –4 |
50–59 | 0.2 | –4 |
60–69 | 0.2 | –4 |
70–79 | 0.6 | –4 |
80–89 | 1.3 | –3 |
Hydrosyringomyelia which occurs in 20–30% of cases.
Cine MRI (CSF flow study)
- May demonstrate blockage of CSF flow at FM.
- Not widely available.
- Accuracy is not high → therefore usually does not alter management.
Myelography
- Generally used only when MRI cannot be obtained.
- Only 6% false negative.
- It is critical to run the intrathecal contrast (dye) all the way up to the foramen magnum.
- Usually combined with CT scan.
Differential
- Vs Chiari type 2
- Chiari 1
- Medulla is not caudally displaced (some authors disagree on this point)
- Brainstem is not involved
- Lower cranial nerves are not elongated
- Upper cervical nerves do not course cephalad.
Management
--- config: layout: dagre --- flowchart TD Chiari1["Chiari 1"] --> Asymptomatic["Asymptomatic<br>"] & Symptomatic["Symptomatic<br>+/- syrinx<br>"] Asymptomatic --> NoSyrinx["No syrinx<br>"] & Syrinx["Syrinx<br>"] NoSyrinx --> ClinSurv["Clinical surveillance<br>"] Syrinx --> ClinSurvMRI["Clinical surveillance<br>+ Interval MRI<br>"] Symptomatic --> RaisedICP["Is there evidence<br>of raised ICP?<br>"] & CVJAnomaly["Is there evidence<br>of CVJ anomaly?<br>"] & MetabolicAnomaly["Is there a metabolic<br>anomaly?<br>"] RaisedICP --> ICPYes["yes<br>"] & ICPNo["no<br>"] ICPYes --> Hydrocephalus["Hydrocephalus<br>"] & Craniosynostosis["Craniosynostosis<br>"] Hydrocephalus --> ConsiderShunt["Consider:<br>ETV/Shunt<br>"] Craniosynostosis --> ConsiderCVP["Consider:<br>Cranial vault procedure<br>"] ICPNo --> FMDecompression["Foramen Magnum<br>decompression<br>"] CVJAnomaly --> CVJYes["yes<br>"] & CVJNo["no<br>"] CVJYes --> AssessCVJ["Assess reducibility<br>and need for cranio-vertebral fixation<br>"] CVJNo --> FMDecompression2["Foramen Magnum<br>decompression<br>"] MetabolicAnomaly --> MetYes["yes<br>"] MetYes --> EvaluateTherapies["Evaluate role<br>of medical therapies"]
Conservative
- Indication
- Asymptomatic patients
- Symptomatic but stable for years
Indications for surgery
- Since patients respond best when operated on within 2 years of the onset of symptoms (see below), early surgery is recommended for symptomatic patients.
- Change of
- Asymptomatic patients → symptomatic
- Symptomatic but stable patients → deteriorating
Surgical techniques
- Extent of craniectomy ()
- Axial:
- 3-4cm or when the foramen magnum becomes vertical
- Sagittal
- 3 cm above the foramen magnum
- A decompression that is too big can lead to cerebellar slumping
- Incision and closure


- Try not to manipulate the tonsils as they have poorer outcomes
- More and more people do just an extradural operation.
- Intraoperature ultrasound is less accurate at predicting those who do not need durotomy in the presence of moderate (below C1 lamina)/severe (below C2 lamina) tonsillar descent.
- Literature
- Klekamp (Germany)
- 492 patients
- Repeat surgery if:
- Large craniectomy
- No arachnoid dissection
- No tonsillar shrinkage
- Autologous duraplasty
- Milhorat (Chiari Institute)
- 2813 patients
- Arachnoid intact
- No tonsillar resection/shrinkage
- Closure of dural defect
- Alexander et al 2019
- 104 (37%) bone-only
- 177 (63%) PFD with duraplasty
- No significant difference in outcomes (p = 0.59)
- Analysis of failures revealed a significant difference in tonsillar coagulation versus those whose tonsils were not manipulated (p = 0.02)
- Thakar et al 2018
- Gait imbalance associated with worse clinical outcome
- Motor deficits associated with poor syrinx resolution
- Lower position of obex correlates with better outcome from surgery
- Sahuquillo et al 1994
- Dural graft (10) improved
- Xie J et al, Zhonghua 2000, China
- Dural Graft (37) 87% had improvement
- Munshi I et al, Neurosurgery 2000, Spain
- Graft (23) 87% improvement, 100% Syrinx reduction
- No graft (11) 73% improvement, 50% Syrinx reduction
- Yundt KD, Paediatric Neurosurgery USA
- No Graft (7) 100% improvement
Operative findings
- Tonsillar herniation is present in all cases (by definition), the most common position being at C1 (62%).
- Fibrous adhesions between dura, arachnoid and tonsils with occlusion of foramina of Luschka and Magendie in 41%.
- The tonsils separated easily in 40%.
Finding | % |
Tonsillar descent | 100 |
Below foramen magnum | 4 |
C1 | 62 |
C2 | 25 |
C3 | 3 |
Unspecified level | 6 |
Adhesions | 41 |
Syringomyelia | 32 |
Dural band (at foramen magnum or C1 arch) | 30 |
Vascular abnormalities¹ | 20 |
Skeletal abnormalities | ㅤ |
Inverted foramen magnum | 10 |
Keel of bone | 3 |
C1 arch atresia | 3 |
Occipitalization of C1 arch | 1 |
Cervicomedullary "hump" | 12 |
- ¹vascular abnormalities: PICA dilated or abnormal course in 8 patients (PICA often descends to lower margin of tonsils); Large dural venous lakes in 3
Surgical complications
- After suboccipital craniectomy plus C1–3 laminectomy in 71 patients, with dural patch grafting in 69, one death due to sleep apnea occurred 36 hrs post-op.
- Respiratory depression was the most common post-op complication (in 10 patients), usually within 5 days, mostly at night.
- Close respiratory monitoring is therefore recommended.
- Other risks of the procedure include:
- CSF leak
- Herniation of cerebellar hemispheres
- Vascular injuries (PICA)
Operative results
- Patients with pre-op complaints of pain generally respond well to surgery.
- Sensation may improve when the posterior columns are unaffected and the deficit is due to spinothalamic involvement alone.
- Rhoton feels that the main benefit of operation is to arrest progression.
- The most favourable results occurred in patients with
- Cerebellar syndrome (87% showing improvement, no late deterioration).
- Worse outcome are
- Presence of atrophy
- Weakness is less responsive to surgery, especially when muscle atrophy is present.
- Ataxia
- Scoliosis
- Symptoms lasting longer than 2 years.
Category | Percentage |
Early improvement of pre-op symptoms | 82% |
Percent of above that relapsed¹ | 21% |
Early improvement of pre-op signs | 70% |
No change from pre-op status | 16% |
Worse than pre-op | 0% |
- ¹these patients deteriorated to pre-op status (none deteriorated further) within 2-3 years of surgery; relapse occurred in 30% with foramen magnum compression syndrome, and in 21% with central cord syndrome.