General information
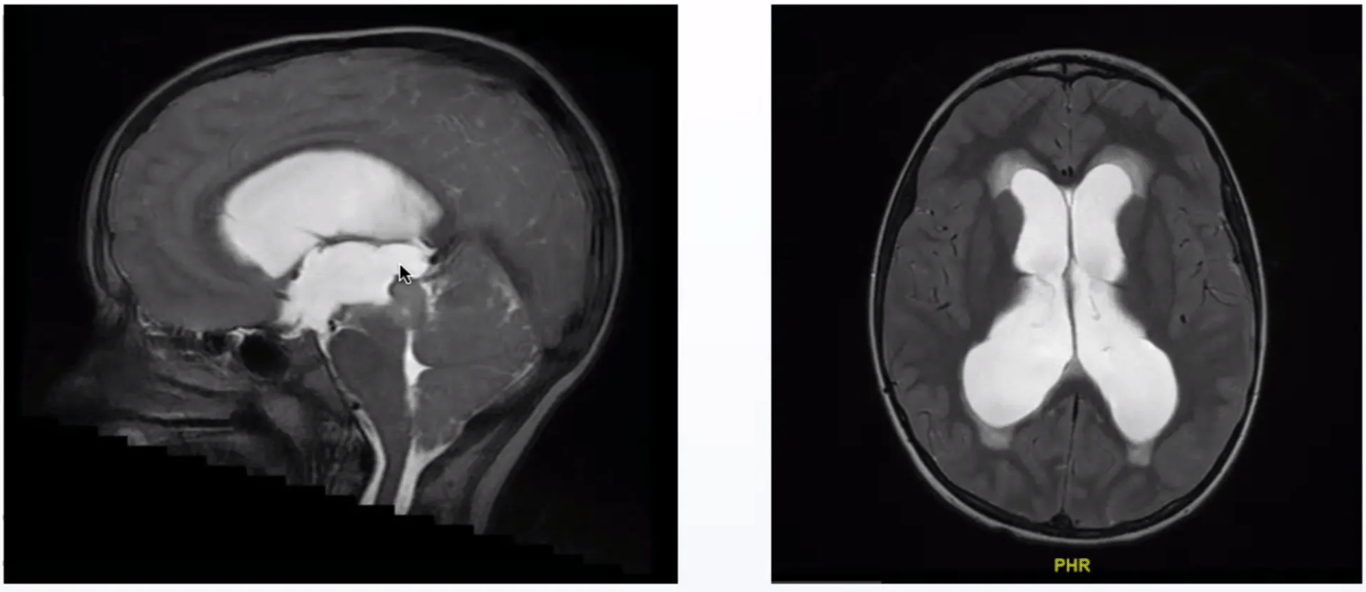
- Aqueductal stenosis (AqS) produces what is sometimes called triventricular hydrocephalus, characterized by a normal sized 4th ventricle and enlarged third and lateral ventricles on MRI or CT.
- Most cases occur in children; however some present for the first time in adulthood.
Aetiologies
- Congenital malformation: may be associated with Chiari malformation or neurofibromatosis
- Acquired
- Inflammation (following haemorrhage or infection, e.g. Syphilis, T.B.)
- Neoplasm:
- Especially brainstem astrocytomas—including tectal gliomas, lipomas
- Quadrigeminal plate arachnoid cysts
Aqueductal stenosis in infancy
- AqS is a frequent cause of congenital hydrocephalus (HCP) (up to 70% of cases), but occasionally may be the result of HCP.
- Patients with congenital AqS usually have HCP at birth or develop it within ≈ 2–3 mos.
- Congenital AqS may be due to an X-linked recessive gene.
- Four types described by Russell:
- Forking:
- multiple channels (often narrowed) with normal epithelial lining that do not meet, separated by normal nervous tissue.
- Associated with other congenital abnormalities
- Spina bifida
- Myelomeningocele
- Periaqueductal gliosis:
- Luminal narrowing due to subependymal astrocytic proliferation
- True stenosis:
- Aqueduct histologically normal
- Septum
Aqueductal stenosis in adulthood
- General information
- AqS may be an overlooked cause of what may be mistaken as “normal pressure hydrocephalus” in the adult.
- It is unknown why some cases of AqS would remain occult, and manifest only in adulthood.
- In one series of 55 cases, 35% had duration of symptoms<1 year, 47% for 1–5 years; the longest was 40 yrs. Although most follow this longstanding benign course, there are reports of elevated ICP and sudden death.
- Symptoms
- Headache
- Most common
- H/A associated with elevated ICP.
- Visual changes
- Blurring or loss of acuity.
- Endocrine changes
- Menstrual irregularities, hypothyroidism, and hirsutism.
- Symptoms of aqueductal stenosis presenting in adulthood (55 patients, > 16 years of age)
Symptom | % |
H/A | 58 |
Visual disturbances | 40 |
Mental deterioration | 31 |
Gait disturbance | 29 |
Frequent falling | 24 |
Endocrine disturbance | 18 |
Nausea/vomiting | 16 |
Seizures | 15 |
Incontinence | 13 |
Vertigo | 11 |
LE weakness | 7 |
Hemiparesis or hemianesthesia | 7 |
Diplopia | 5 |
- Signs
- Papilledema was the most common finding (53%).
- Visual fields
- 22%
- Reduced peripheral vision, increased blind spots, quadrantic or hemianopic field cuts, or scotomata.
- Intellectual impairment
- 36%.
- Other signs included:
- ataxia (29%),
- “pyramidal tract signs” in 44%
- mild hemi- or para-paresis (22%)
- spasticity (22%),
- Babinski’s (20%),
- Anosmia (9%)
- Evaluation
- MRI CISS and CSF Flow studies
- Demonstrates the absence of the normal flow void in the Sylvian aqueduct.
- MRI + Contrast
- R/O tumor.
Treatment (of non-tumoral AqS)
- Options
- Shunting:
- Torkildsen shunt (shunting a lateral ventricle to the cisterna magna) may work in adult cases; however, pediatric patients with obstructive hydrocephalus may not have an adequately developed subarachnoid space for this to function properly
- ETV
- Follow-up of at least two years to rule out tumor is recommended.