Definition
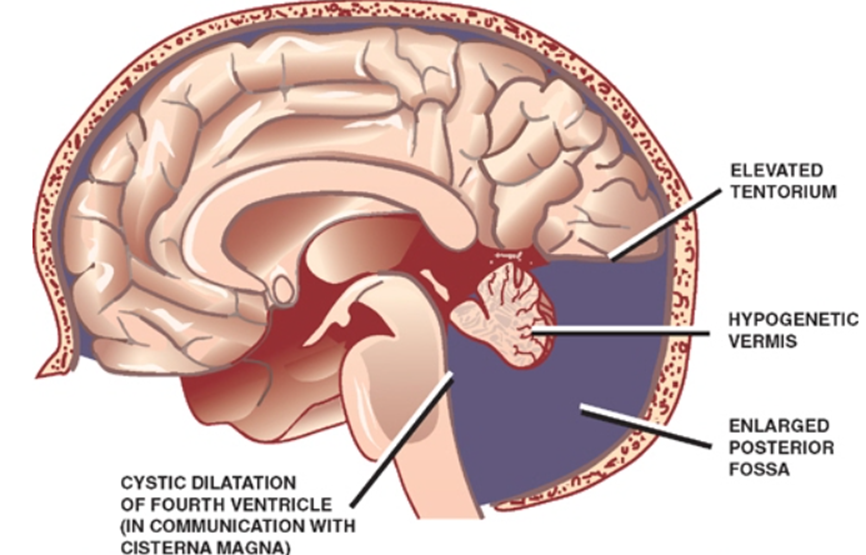
- agenesis or hypoplasia of the cerebellar vermis
- cystic dilation of the fourth ventricle, (encased in a neuroglial vascular membrane)
- not posterior fossa subarachnoid space
- Not arachnoid cyst;
- enlargement of the posterior fossa with or without hydrocephalus
- Due to cystic dilatation of 4th ventricle
- Elevated tentorial attachment
- Due to cystic dilatation of 4th ventricle
Numbers
- Present in 2–4% of all cases of hydrocephalus
- Incidence: 1 per 25,000–35,000 live births
- M:F = 1:3.
- May be associated with PHACES syndrome
Aetiology
- Gestational exposure to
- Rubella
- CMV
- Toxoplasmosis
- Warfarin
- Alcohol
- Isotretinoin
- Autosomal recessive inheritance has been identified in a few cases, but a genetic basis is lacking in most.
- May be associated with PHACES syndrome (p.1443).
Mech
- Unknown cause
- Due to dysembryogenesis of the roof of the rhombencephalon → agenesis of the cerebellar vermis with a large posterior fossa cyst communicating with an enlarged 4th ventricle
- Not due to failure of formation of the 4th ventricle
- a complex disruption of the interaction between the developing cerebellum and the developing posterior fossa mesenchyme and its derivates.
Clinical presentation
- Macrocephaly
- 90%–100% of children during the first months of life
- Hydrocephalus (70-90%)
- Associated abnormalities
- CNS abnormalities
- agenesis of the corpus callosum in 17%,
- occipital encephalocele in 7%.
- Other findings include
- heterotopias,
- spina bifida,
- syringomyelia,
- microcephaly,
- dermoid cysts,
- porencephaly, and
- Klippel-Feil deformity.
- Most have an enlarged posterior fossa with elevation of the torcular herophili.
- Atresia of the foramina of Magendie and Luschka may occur.
- Systemic abnormalities:
- facial abnormalities (e.g. angiomas, cleft palates, macroglossia, facial dysmorphia),
- ocular abnormalities (e.g. coloboma, retinal dysgenesis, microphthalmia), and
- cardiovascular anomalies (e.g. septal defects, patent ductus arteriosus, aortic coarctation, dextrocardia)
- be aware of the possibility of a cardiac abnormality when considering surgery on these patients.
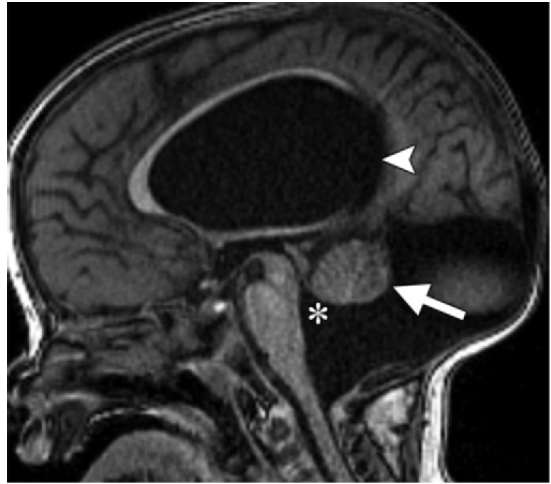
Imaging
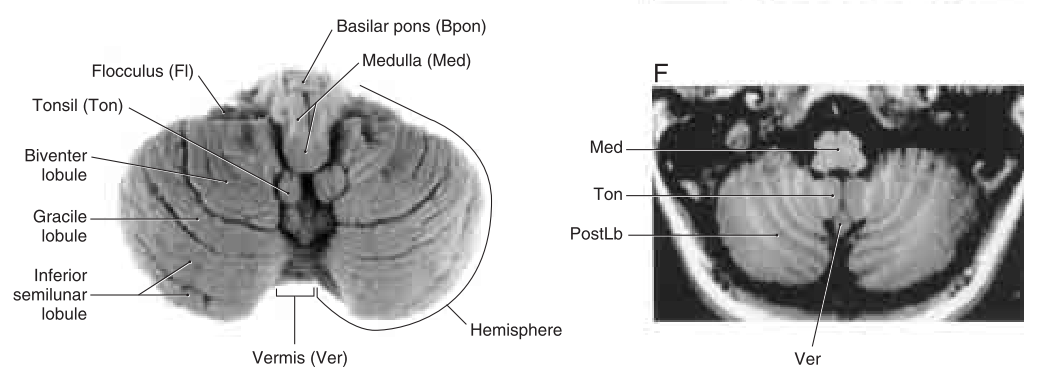
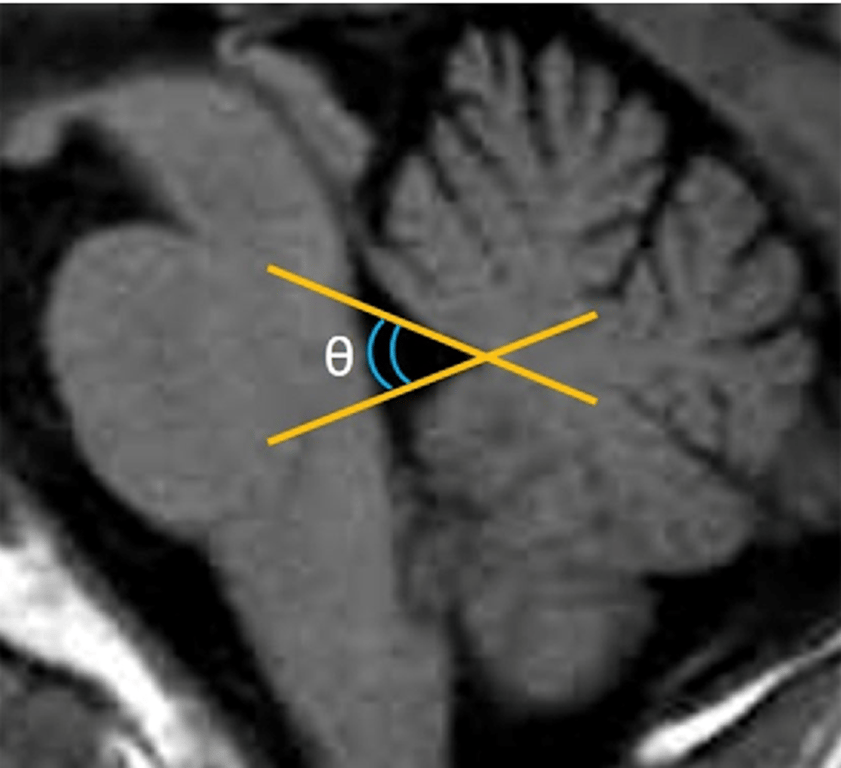
Normal vermis
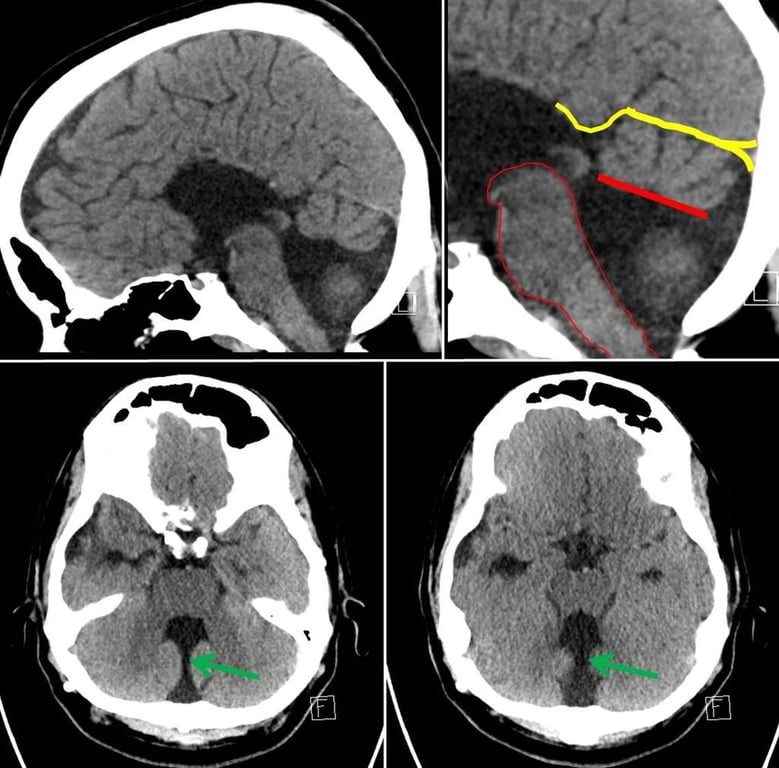
6 radiographic features necessary for diagnosis:
- a large posterior fossa cyst communicating with the fourth ventricle
- absence of a portion of the inferior vermis
- hypoplasia, anterior rotation, and upward displacement of the remaining vermis
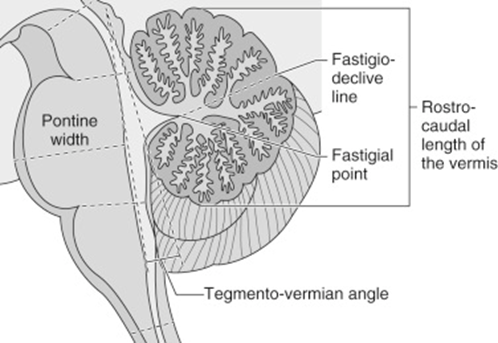
- absence or flattening of the angle of the fastigium
- a large posterior fossa with torcular elevation
- anterolateral displacement of the cerebellar hemispheres
USS
- 3 findings
- marked enlargement of the cisterna magna (≥10 mm)
- complete aplasia of the vermis
- a trapezoid-shaped gap between the cerebellar hemispheres
- Antenatal ultrasound may falsely overdiagnose the condition if performed before 18 weeks, as the vermis has not properly formed.
MRI
- 3 findings
- hypoplasia of the vermis and cephalad rotation of the vermian remnant
- cystic dilatation of the fourth ventricle extending posteriorly; usually the cerebellar hemispheres are displaced anterolaterally, but with a normal size and morphology
- enlarged posterior fossa with torcular-lambdoid inversion (torcular lying above the level of the lambdoid due to abnormally high tentorium)
Treatment:
- Hydrocephalus
- Early treatment to achieve maximum cognitive development.
- No hydrocephalus, DWM may be followed and if require surgery then:
- Shunting
- Posterior fossa cyst must be shunted.
- Do not shunt lateral ventricles alone (contraindicated): Risk of upward herniation.
- It is important to confirm patency of the cerebral aqueduct, otherwise the supratentorial ventricles need to be shunted concurrently.
- Varying reports exist regarding rates of associated aqueductal stenosis, although it is widely believed to be rare.
- Excision of the obstructing membrane.
- High risks of morbidity and mortality.
- Option for patients with frequent shunt malfunctions.
- ETV
- If aqueduct is not patent
- however, further study is necessary for its effectiveness
Prognosis
- Prognosis ranges widely as there are various levels of severity of the malformation.
- 12–50% mortality rates, although this is improving with modern shunting techniques.
- Only 50% have normal IQ.
- Ataxia, spasticity, and poor fine motor control are common.
- Seizures occur in 15%.