General
- Dysraphism = incomplete fusion
Various classification
Lemire classification (embryological classification)
Gastrulation disorder
- Notes: Trilaminar disc formation, abnormalities will be ventrally placed and involved all layers of germ cell (skeletal anomalies are common)
- Split cord malformation (Formation of accessory neuroenteric canal)
- Diastematomyelia
- Diplomyelia
- Neurenteric cysts
- Persistence of neurenteric canal of kovalevsky
- Klippel-Feil syndrome
- Dermoid, Epidermoid cyst
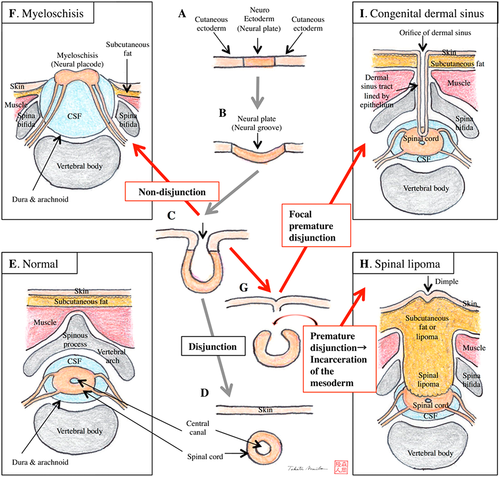
Neurulation defects
- Notes: non-closure of the neural tube results in open lesions
Primary neurulation disorder
- Craniorachischisis:
- Total dysraphism
- Many die as spontaneous abortion
- Disjunction disorder
- Non disjunction
- Myelomeningocele
- Open Neutral tube defects
- Due to disruption of the infolding of the neural plate to form the neural tube → overlying mesodermal and ectodermal elements fail to form → open spinal defect
- Neuro placode: Disruptions of the infolding process of neural plate into neural tube causes a persistent neural plate
- Meningocele
- Myeloschisis
- Premature disjunction
- Limited dorsal myeloschisis
- Dermal sinus tract
- Spinal lipomas Type 1
Junctional disorder
- Spinal lipomas Type 2 (Lipomyelomeningocele)
Secondary Neurulation disorder (ONLY CONDITION where the spinal cord terminates high)
- Spinal lipomas
- Type 3: Lipomyelomeningocele
- Type 4
- Dermal sinus tract
Postneurulation defects
- Notes: Produces skin-covered (AKA closed) lesions (some may also be considered “migration abnormalities”; see below)
- Cranial
- Encephalocele
- Meningocele
- Chiari II malformation
- Migration abnormalities
- Microcephaly
- Hydranencephaly
- holoprosencephaly
- Porencephaly
- Agenesis of corpus callosum
- Cerebellar hypoplasia/Dandy Walker syndrome
- Macroencephaly
- Spinal
- hydromyelia/syringomyelia
Dysraphism
Type | Description | Stage Affected |
Open spinal dysraphism | ㅤ | ㅤ |
Myelomeningocele | Defect in dura, posterior vertebral elements, facia and skin causing the neural placode to be exposed in the midline | Primary neurulation |
Myelocele | As myelomeningocele, but subarachnoid space ventral to placode is not expanded resulting in a lesion flush with skin | |
Hemimyelocele | Myelocele affecting one of two hemicords in split cord malformation | Gastrulation and primary neurulation |
Hemimyelomeningocele | Myelomeningocele affecting one of two hemicords in split cord malformation | |
Closed spinal dysraphism with subcutaneous mass | ㅤ | ㅤ |
Lipomyelomeningocele | A subcutaneous lipoma tethers the spinal cord (lipoma-placode interface) outside the spinal canal via defect in vertebral elements | Primary neurulation |
Lipomyelocele | A subcutaneous lipoma tethers the spinal cord (lipoma-placode interface) inside the spinal canal via defect in vertebral elements | |
Meningocele | Posterior—Herniation of CSF-filled meningeal sac through posterior bony defect (may contain nerve roots but not spinal cord). Dura may have defect but overlying skin is intact. Anterior meningoceles are part of the caudal regression syndrome | Unknown |
Terminal myelocystocele | Expansion of terminal central canal (syringocele) surrounded by a meningocele with no communication between two components. Syringocele is caudal to the meningocele and herniates through a wide spina bifida to cause a intergluteal cystic swelling | Secondary neurulation and retrogressive differentiation |
Closed spinal dysraphism without subcutaneous mass | ㅤ | ㅤ |
Simple dysraphic state | ㅤ | ㅤ |
Posterior spina bifida | Simple defect of fusion of posterior neural arch of a vertebra, usually at L5 or S1 | |
Intradural lipoma | Lipomas originate from early disjunction between neuroectoderm and ectoderm | Primary neurulation |
Filum terminale lipoma | Fibrolipomatous thickening of the filum terminale | Secondary neurulation and retrogressive differentiation |
Tight filum terminale | A short thick filum (> 2 mm without fat), which impairs the ascent of conus medullaris. | |
Persistent terminal ventricle | Small ependymal lined cavity in the conus medullaris which may undergo cystic dilatation | |
Complex dysraphic state | ㅤ | ㅤ |
Split cord malformation | Type 1—bony midline septum dividing cord into two separate cords in own dural sleeves Type 2—single thecal sac containing split cords with an intervening fibrous band | Gastrulation (notochordal integration) |
Neuroenteric cyst | Cysts usually in intradural extramedullary plane of endodermal origin, usually lined with GI or respiratory epithelium | |
Dorsal enteric fistula | Most severe. Cleft connecting the bowel with dorsal skin surface through the prevertebral soft tissues, split vertebral bodies and spinal cord, neural arch, subcutaneous tissue | |
Dermal sinus | Epithelium-lined fistula which extends from skin to meninges within the spinal canal, possibly opening into the subarachnoid space or connecting to filum terminale, lipoma and may also be associated with a spinal dermoid | |
Caudal regression syndrome | Agenesis of spinal column, imperforate anus, genital anomalies, bilateral renal dysplasia, pulmonary hypoplasia and lower limb abnormalities. Syndromic associations include OEIS, VACTERL and Currarino triad | Gastrulation (notochordal formation) |
Currarino triad | sacral agenesis abnormalities anorectal malformation presacral mass consisting of teratoma, anterior sacral meningocele or both | |
VACTERL | V - Vertebral anomalies-Congenital scoliosis A - Anorectal malformations C - Cardiovascular anomalies T - Tracheoesophageal fistula E - Esophageal atresia R - Renal (Kidney) and/or radial anomalies L - Limb defects | |
Segmental dysgenesis | Segmental agenesis of thoracolumbar spine: vertebral, segmental spinal cord hypoplasia/aplasia with caudal bulkiness, congenital paraparesis, lower limb deformities |