Definition
- A spinal dysraphism due to abnormalities in primary and/or secondary neurulation where fat is abnormally located on the cord, conus or filum
Background
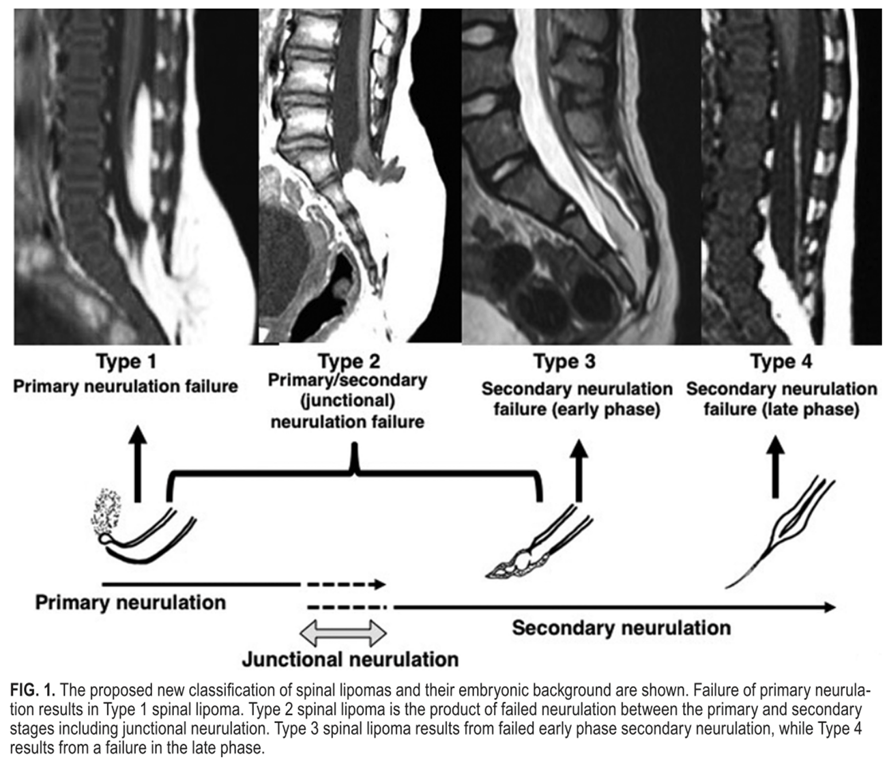
- The embryonic background of spinal lipoma cases is marked by a premature disjunction between the neural and cutaneous ectoderm during the process of primary neurulation.
- Failed primary neurulation allows invasion of mesenchymal tissue of mesodermic origin into the neural structure, leading to the formation of a spinal lipoma.
- An unfused spinal cord caused by failed primary neurulation remains dysraphic in spinal lipoma.
- Embryologists often consider closed spinal lesions to be the result of failed secondary neurulation.
- Indeed, the presence of a lipoma in the filum terminale, the final product of secondary neurulation, is increasingly being acknowledged. The availability of MRI has made the discovery of caudally located lipomas, which do not penetrate the dorsal aspect of the dura mater or fascia, and are unassociated with spina bifida, more common.
- It should be remembered that spina bifida diagnosed in such patients does not constitute true "pathological" spina bifida, but merely "physiological spina bifida" formed by the cartilaginous part of the lamina in the course of normal development.
- Surgically orientated classification of spinal lipoma was first proposed by Chapman and underwent various modifications based on MRI findings.
- Chapman's classification is still useful today but does not account for spinal lipomas originating from failed secondary neurulation. Some have included the filum lipoma in the classification. However, because this classification is simply based on the site and morphology of the spinal lipoma, it is now considered to have less clinical significance.
Classification
- Has various forms but only 3 are clinically important: Because they can cause Tethering and Compression
- Lipomyelocele/lipomyelomeningocele: 84%
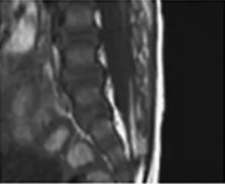
- Lipoma of the filum terminale: 12%
- Intradural lipoma: 4%
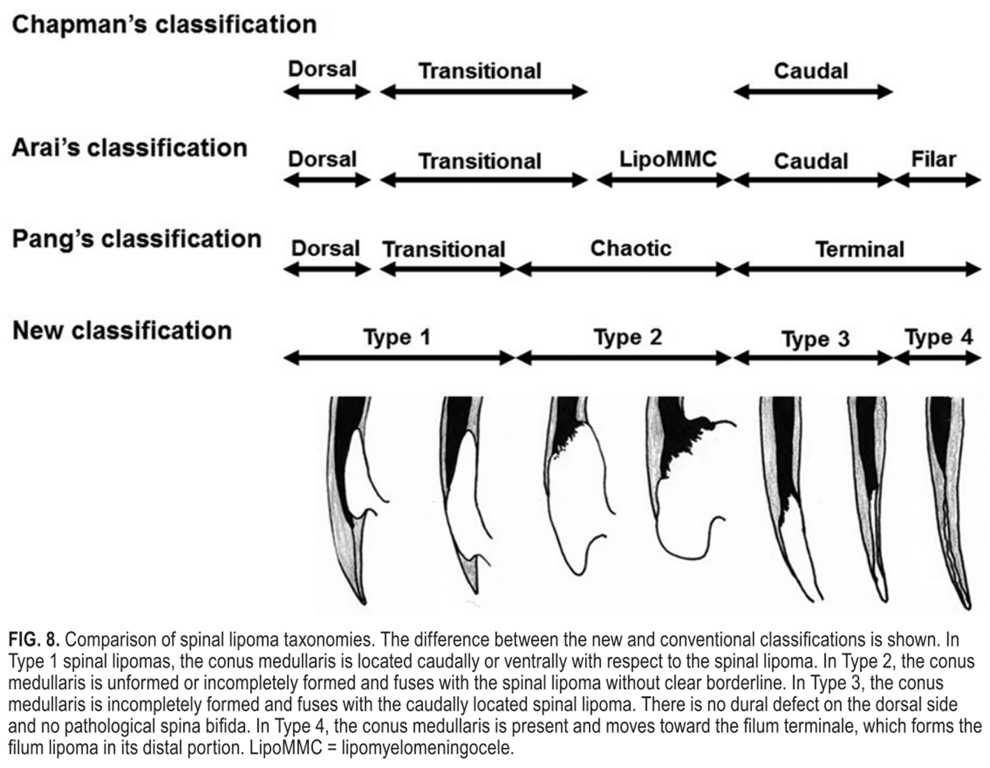
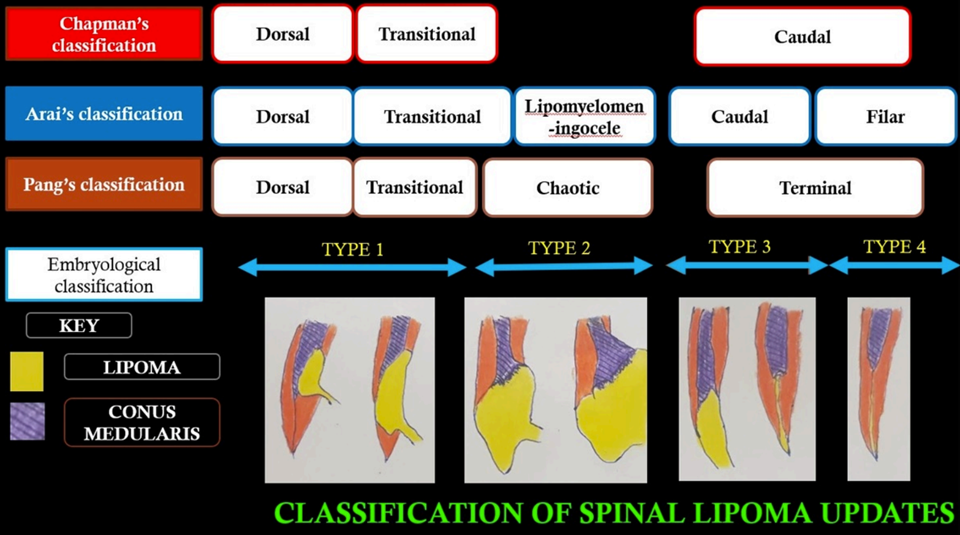
New: Morata et al based on embryological stages
- Types of spinal lipoma
- Clinical findings - Skin stigmata; fascial and dural defect
- Spina bifida - Pathological spina bifida
- Timing of diagnosis - Neonatal period
- Relationship with conus medullaris - Dorsal location predominant with some uneven lateral extension
- Surgical implications - Not easy, but not extremely difficult; radical resection possible
- Associated anomalies - Usually none
- Clinical findings - Skin stigmata; fascial and dural defect
- Spina bifida - Pathological spina bifida
- Timing of diagnosis - Neonatal period
- Relationship with conus medullaris - Dorsal to lateral, partly ventral extension with neural elements inside not unusual
- Surgical implications - Difficult; radical resection impossible
- Associated anomalies - Anorectal/sacral anomalies can be seen
- Clinical findings - No or only tiny skin stigmata; no dorsal dural defect
- Spina bifida - Physiological spina bifida
- Timing of diagnosis - Late infancy or school age (not unusual)
- Relationship with conus medullaris - Caudal to conus medullaris, but without clear borderline; lateral, ventral extension not unusual
- Surgical implications - Moderately difficult in some cases; radical resection not indicated
- Associated anomalies - Anorectal/sacral anomalies often seen
- Clinical findings - Tiny skin stigmata (dimple)
- Spina bifida - Physiological spina bifida
- Timing of diagnosis - Infancy
- Relationship with conus medullaris - Normal conus medullaris, lipoma of the filum terminale
- Surgical implications - Simple and usually straightforward
- Associated anomalies - Anorectal/urogenital anomalies not unusual
Type 1 - Pure primary neurulation failure

Type 2 - Ranging from primary to secondary neurulation failure

Type 3 - Secondary neurulation failure (early phase)

Type 4 - Secondary neurulation failure (late phase)

OLD: Chapman et al + Pang et al
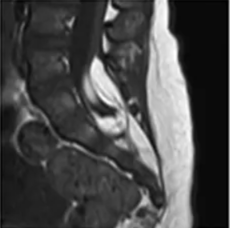
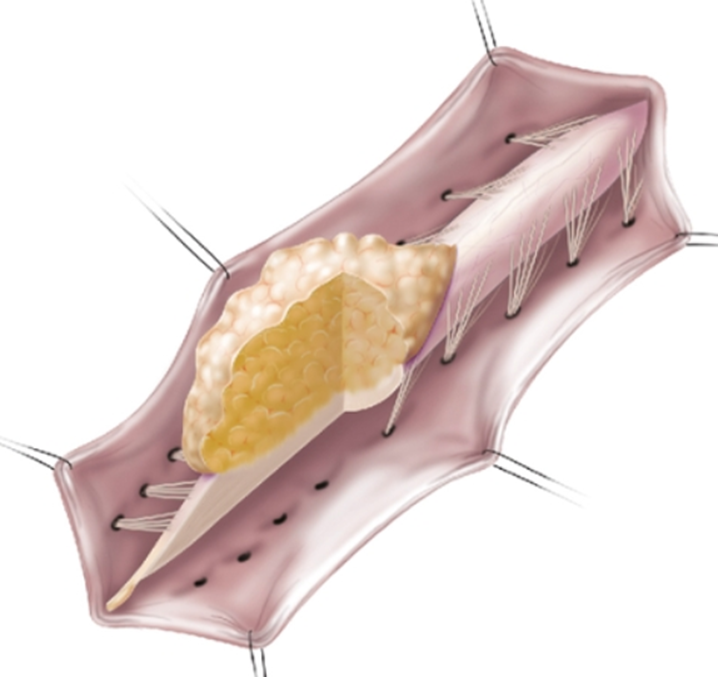
Terminal (caudal)
- lipoma–spinal cord interface is located at the caudal end of the conus, almost like a continuation of the spinal cord itself
- Mainly lateral s(x)
- nerve roots may lie ventral to the lipoma or pass through the mass itself.
- Diffuse interface
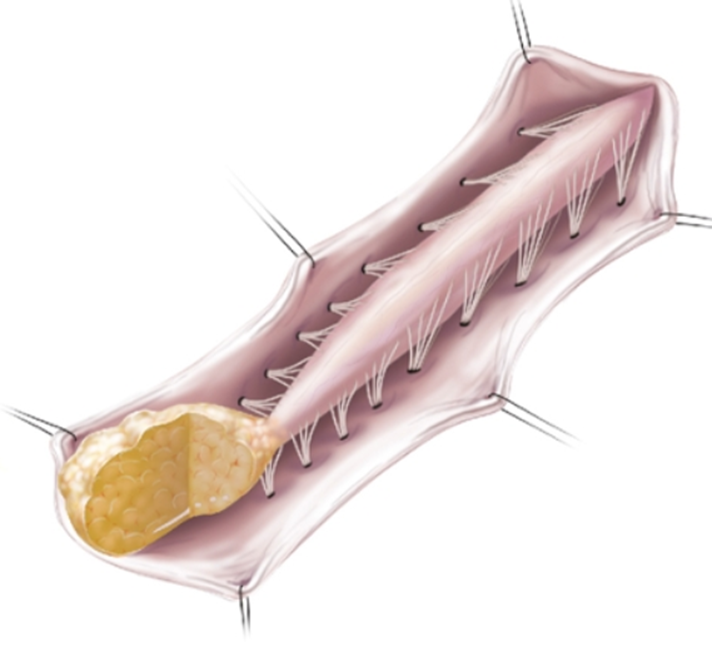
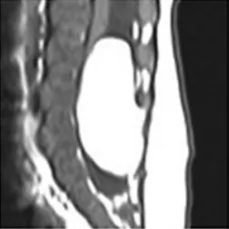
Dorsal
- Lipomas insert onto the dorsal surface of the conus medullaris
- Mainly midline s(x)
- Substantial subcutaneous fat component attached to the underlying spinal cord via a fibrolipomatous stalk of varying thickness.
- Discreet interface
- Midline interface
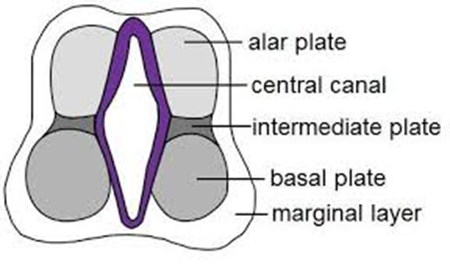
- posterior half of the lower spinal cord at the site of neural fold fusion is unfused (i.e., a partial dorsal myeloschisis is present)
- the stalk attaches directly to the exposed alar and basal cord regions, just posterior and medial to the posterior columns and dorsal to the central canal
- No evidence of leptomeninges posteriorly, and no sensory or motor roots are found within the actual substance of the lipoma.
- Lateral interface
- Sensory nerve roots emerge just anterior to lateral line of fusion,
- Sensory nerve roots can be traced circumferentially.
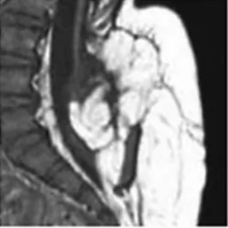
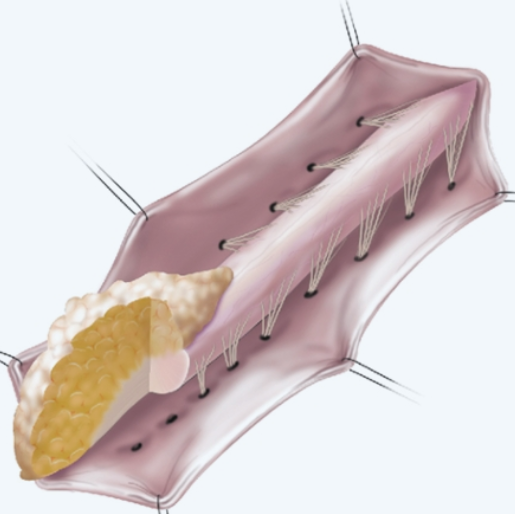
Transitional (between the two)
- Cephalad portion:
- Dorsal type
- Posterior rootlets emerging from the cord just ventral to the line of fusion of the lipoma to the cord and leptomeninges.
- Caudal portion:
- Terminal type
- line of fusion is displaced ventrally, nerve roots emerge from within the anterolateral portion of the lipoma mass.
Chaos (Pang et al)
- LMM begins dorsally in an orderly fashion, but its caudal portion is ventral to the neural placode, engulfing neural tissue and nerve roots.
- Fusion line
- Rostral: Distinct
- Caudal: Blurred
- Making the location of the dorsal root entry zone and nerve roots less predictable and surgical resection difficult.
- Chaotic lipomas are uncommon
- Associated with sacral agenesis.
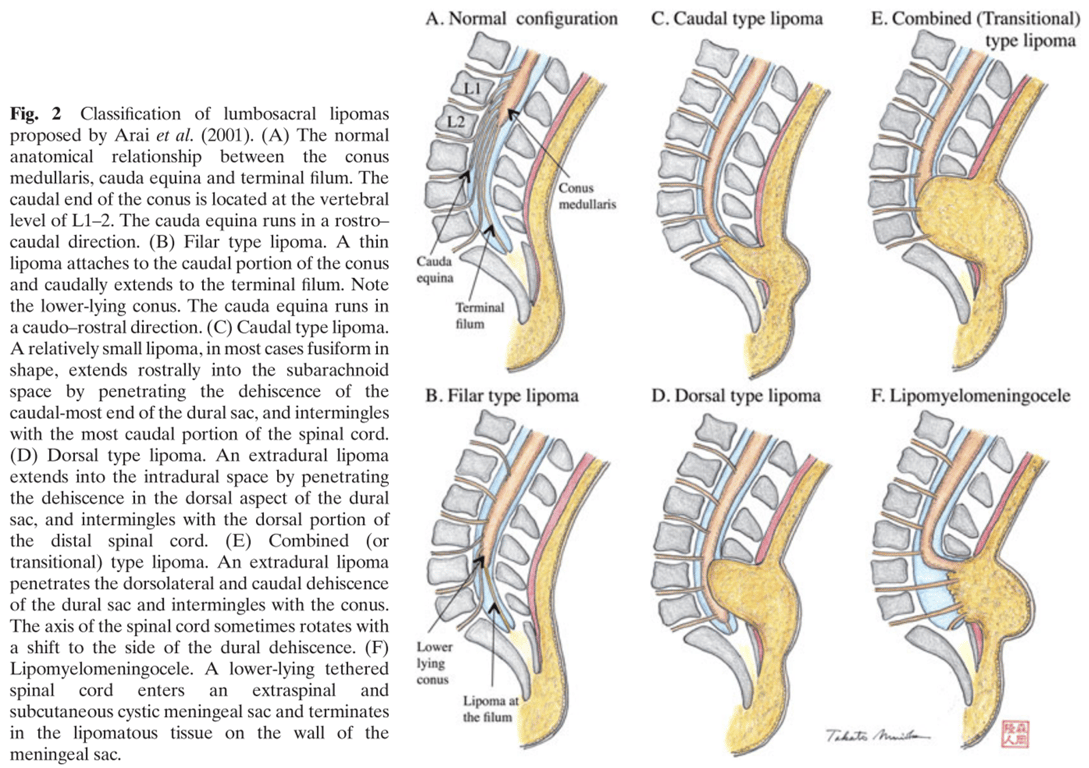
OLD: Arai et al