Definition
- A tract beginning at the skin surface, lined with epithelium. Usually located at either end of neural tube: cephalic or caudal.
- Most common location is lumbosacral
Pathogenesis
- Formed during the 3rd-5th fifth weeks
--- config: layout: dagre --- flowchart TD A["Incomplete disjunction<br>between cutaneous and<br>neural ectoderms"] --> C C["Formation of<br>epithelial-lined sinus tract"]
- Difference
- vs Encephalocele where the primary neurulation has occured and disjunction has completed sucessfully but there is a defect in the skull causing the intracranial contents to herniate
- vs Limited Dorsal Myeloschisis which is non epithelial lined tract
Pathology
- Tract
- Starts at intradural space
- End in Subcutaneous tissue or in any tissue plane superficial to the intradural space.
- Wall
- Lined by stratified squamous epithelium.
- Contents of sinus tract frequently contains elements of both (Because the primitive ectoderm has the capacity to form both)
- Dermal tissue: hair follicles, sebaceous glands, and sweat glands
- Epidermal tissue: Stratified squamous epithelium
- Associated dermoid or epidermoid cysts
- May form at any point along the sinus tract
- Most commonly at the terminus of the tract.
Location
- Midline
- Anywhere between nasion and coccyx
- Not commonly found between the glabella and the inion
Clinical presentation (varies)
- Benign cutaneous cosmetic blemish
- Serious intracranial infection
- Tumour-like process due to mass effect from a dermoid or epidermoid cyst
- Commonly associated cutaneous stigmata
- Angiomata
- Abnormalities of pigmentation
- Hypertrichosis
- Abnormal hair pattern
- Subcutaneous lipomata
- Skin tags
Spinal dermal sinus
Numbers
- 1/1500 births
Clinical presentation
- Dimple or Sinus
- Opening of only 1–2mm
- with or without hairs
- very close to midline
- Surrounding skin
- Normal
- Pigmented (“port wine” discoloration)
- Distorted by an underlying mass.
- The end of the sinus
- Terminate superficially
- Connect with the coccyx, or
- Traverse between normal vertebrae or through bifid spines to the dural tube.
- If the tract expands intrathecally to form a cyst, the mass may present as a tethered cord or as an intradural tumor.
- Incidence of a presumed sacral sinus (a dimple whose bottom could not be seen on skin retraction): 1.2% of neonates
- The course of the sinus

- Bladder dysfunction is usually the first manifestation.
- The tract from a spinal dermal sinus always courses cephalad as it dives inward from the surface
5 major problems
- Tethering of the spinal cord : bladder and bowel dysfunction,
- Bacterial meningitis
- Aseptic (chemical) meningitis
- Compression of the spinal cord or nerve roots from a dermoid cyst.
- Diastematomyelia
Cyst formation: May widen at any point along its path to form a cyst;
Epidermoid cyst
- Lined with stratified squamous epithelium
- Containing only keratin from desquamated epithelium
Dermoid cyst
- Lined with stratified squamous epithelium and dermis
- Containing
- Skin appendages (hair follicles and sebaceous glands)
- Containing sebum and hair.
Complication
- Meningitis
- A potential pathway for intradural infection → meningitis (recurrent) and/or intrathecal abscess.
- Cellulitis
- Chemical (sterile) meningitis
- Less serious,
- Irritation from contents of the sinus tract → sterile (chemical) meningitis with possible delayed arachnoiditis if it enters the dural space.
Dermal sinuses are similar but distinct from pilonidal cysts, which may also be congenital
- (although some authors say they are acquired), contain hair, are located superficial to the postsacral fascia, and may become infected.
Evaluation
- These tracts are NOT to be probed or injected with contrast as this can precipitate infection or sterile meningitis.
- Exam is directed towards detecting abnormalities in sphincter function (anal and urinary), lumbosacral reflexes, and lower extremity sensation and function.
- Radiological
- U/S
- Best modality at birth,
- MRI
- Sagittal images may demonstrate the tract and its point of attachment.
- Easily demonstrates masses (lipomas, epidermoids…) within the canal.
- Plain X-rays must be done when embarking on surgery as part of operative planning, as preparation for the possibility of a complete laminectomy.
Treatment
Indications
- Sinuses above the lumbosacral region should be surgically removed.
- More caudally located sinuses are slightly controversial.
- Although ≈ 25% of presumed sacral sinuses seen at birth will regress to a deep dimple on follow-up (time not specified), it is recommended that all dermal sinuses should be surgically explored and fully excised prior to the development of neurologic deficit or signs of infection.
- The results following intradural infection are never as good as when undertaken prior to infection.
- Sinuses that terminate on the tip of the coccyx rarely penetrate the dura, and may not need to be treated unless local infection occurs.
Timing of surgery
- Surgery within the week of diagnosis is appropriate.
Surgical technique
- An ellipse is cut around the opening, and the sinus is followed deep until the termination of the tract is encountered.
- Careful insertion of a lacrimal duct probe under direct vision may facilitate excision without violating the tract.
- If the tracts penetrates the spine, laminectomy must be performed and the tract followed to its full extent (even if necessary to extend the laminectomy to T12).
- An extradural cyst may be present.
- If the tract enters the dura, it usually does so in the midline, and in these cases the dura should be opened and inspected. Extreme care is taken to prevent spilling cyst contents into the subdural space.
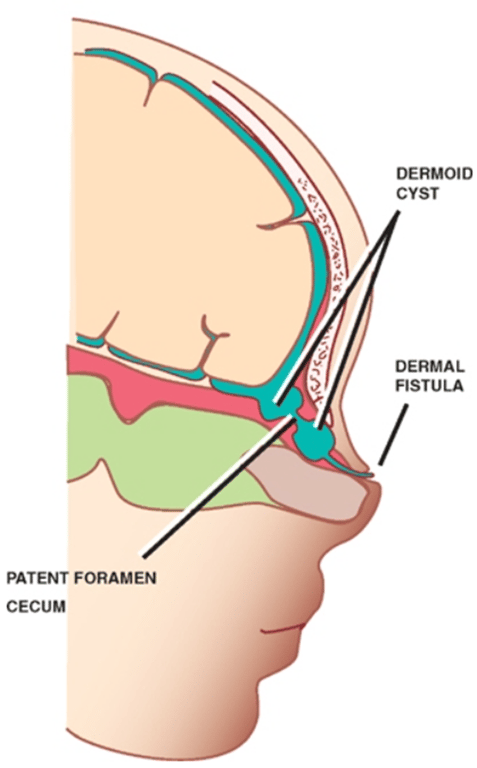
Cranial dermal sinus
Clinical presentation
- Meningitis
- Infective meningitis (Recurrent)
- Bacterial (usually S. aureus)
- Aseptic meningitis
- Stalk begins with a dimple in the occipital or nasal region.
- Cutaneous stigmata:
- Haemangioma
- subcutaneous dermoid cyst
- abnormal hair formation
- Occipital sinuses extend caudally, and if they enter the skull, they do so caudal to the torcular haemophili
Evaluation
- MRI to look for intracranial extension and associated anomalies, including an intracranial dermoid cyst.
Treatment
- A sagittal based incision to permit deep exploration.
- The tract must be followed completely.
- Be prepared to enter the posterior fossa.