General
- Vs Open neural tube defect
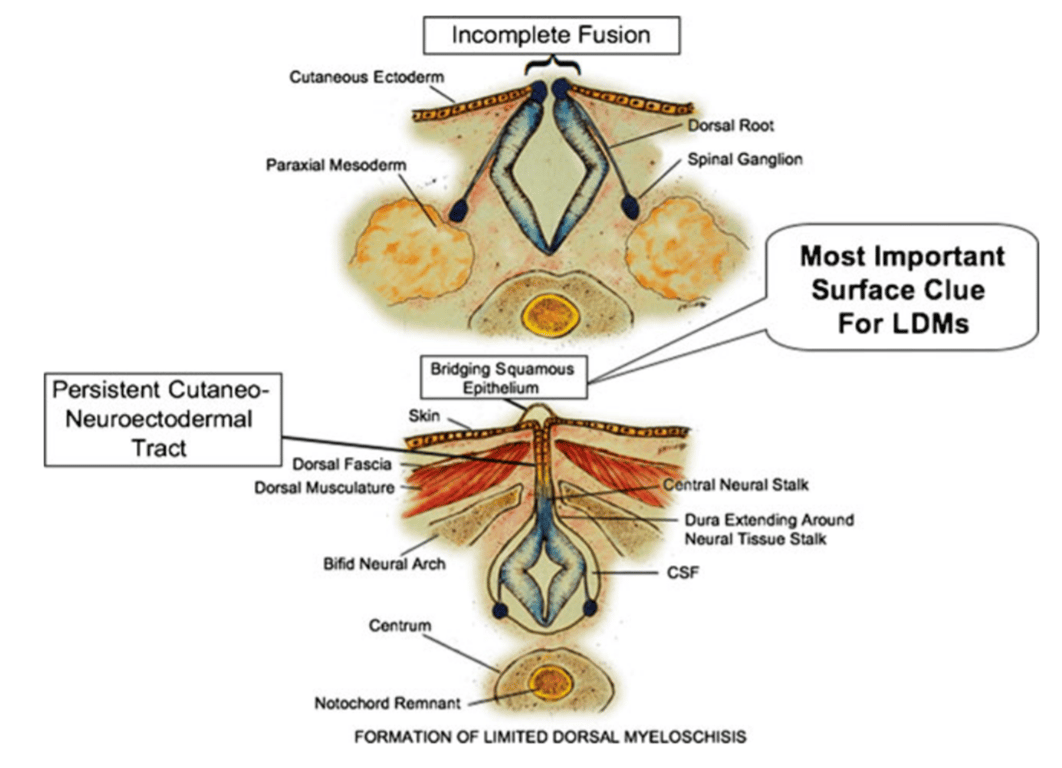
- A less extreme form (when compared to Open neural tube defects), without an overtly unfused (unneurulated) and exposed neural plate but still containing, as its central feature, a small, segmental, and confined area of incomplete dorsal closure of the neural folds
- Open neural tube defect is an extreme form of primary neurulation failure with complete absence of dorsal elevation and midline dorsal fusion (neurulation) of the primary neural plate
Numbers
- Mean age of 5.6 years
Location
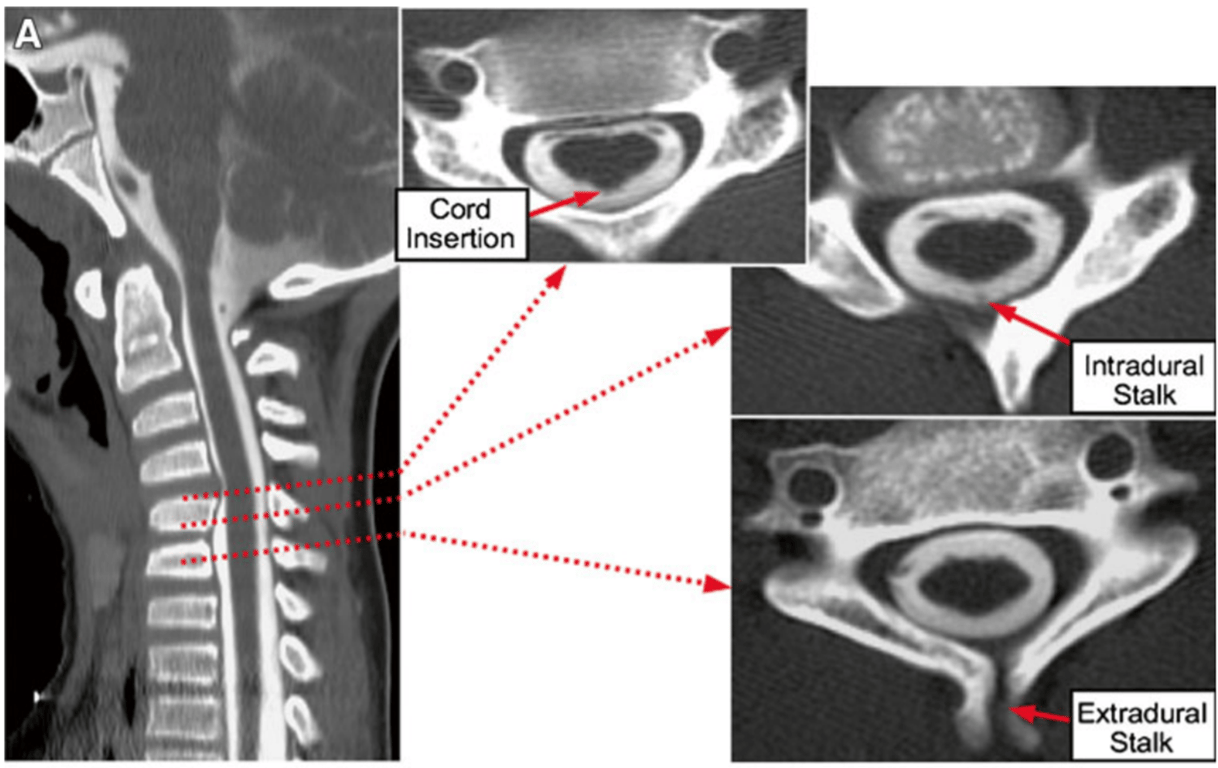
- The vertebral level where the stalk joins the spinal cord
- Mainly lower thoracic
Mechanism
--- config: layout: dagre --- flowchart TD A["Incomplete disjunction<br>between cutaneous and<br>neural ectoderms"] --> C["Formation of<br>fibroneural stalk without<br>epithelial lining<br>from skin to dorsal<br>spinal cord"] B["Incomplete fusion<br>of the neural<br>folds at the midline"] --> C
- A persistent cutaneo-neuroectodermal tract maintains a physical link between the cutaneous margin of the limited skin defect and the dorsal midline spinal cord.
- Ensheathed by a dural extension from the thecal sac as dura forms around the cord, is present in every LDM and is an internal hallmark.
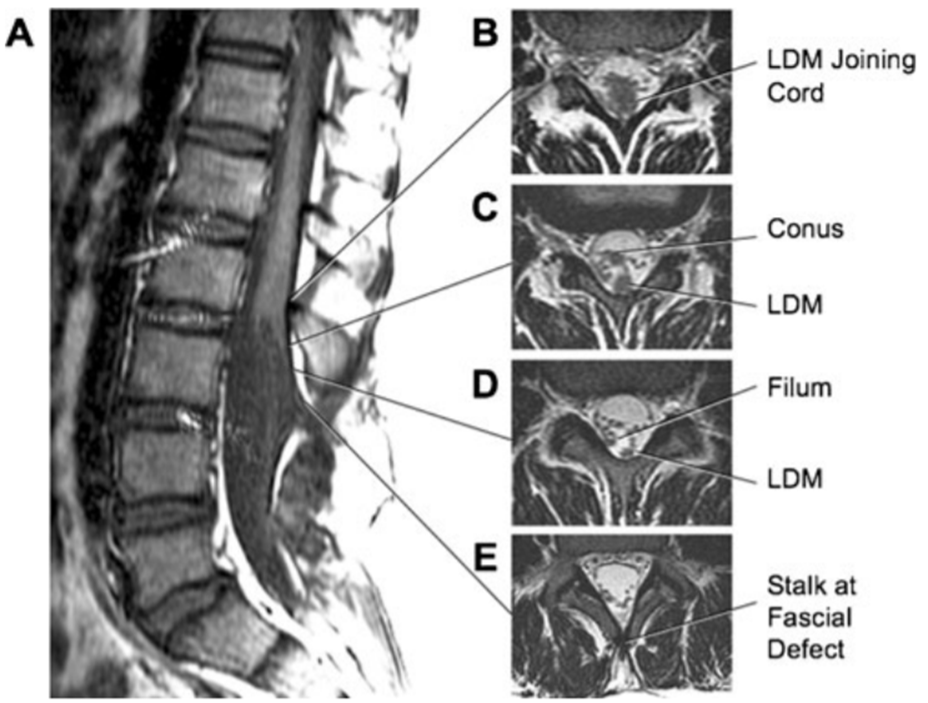
- The cord is often tented up and tethered by this stalk.
- The initially unfused midline integument is subsequently closed by a bridging layer of squamous epithelium that is not full-thickness skin.
- This midline “non-skin” coverage is the external hallmark of an LDM
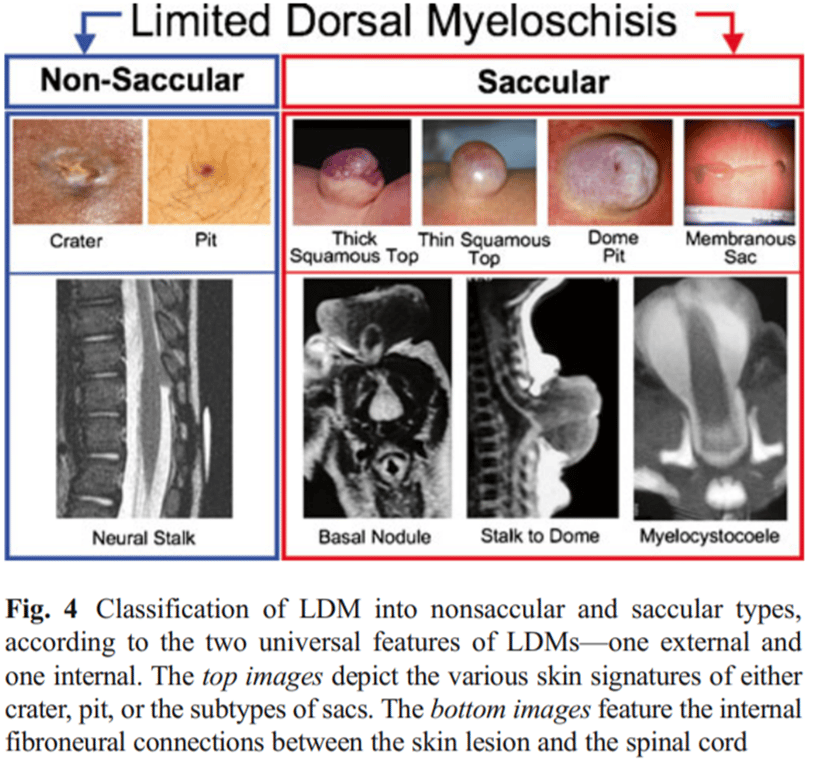
Classification
Clinical features
- The defining external or cutaneous signature always involves a focal area not of normal full-thickness skin, in two forms (midline crater or pit on a flat surface OR on the dome of a saccular swelling)
- Most flat craters are small and discrete, but the occasional saccular bulge can be obtrusive.
- The defining internal structure is always a neatly circumscribed stalk connecting the base of the skin lesion to a ‘‘limited’’ locus on the dorsal midline of the underlying spinal cord.
- At least part of the connection contains central nervous system tissue, qualifying it as a fibroneural or fibrovasculoneural stalk, depending on the accompanying elements.
- The connecting stalk is always ensheathed in a slender dural fistula extending from the site of the stalk’s attachment on the dorsal spinal cord to the base of the skin lesion and sometimes beyond.
Radiology
Treatment
- Surgery
- Indication
- Determined by whether a saccular lesion has become a major hindrance to proper handling of the infant.
- Large sacs operated within 1-2 months of birth
- Small sacs and flat skin lesions are usually operated on at 4–9 months of age to avoid complications associated with surgery on newborns.
- Given the non-leaking nature of LDMs (except in the two cases of ruptured membranous sac), the argument for urgent surgery to prevent infection is not tenable
- Goal
- Removing the tethering effect on the cord exerted by the fibroneural stalk
- Surgical technique check the attached paper by Pang 2013 et al
DDx
- LDM vs CDS: Lee et al 2017
Features | Limited dorsal myeloschisis | Congenital dermal sinus |
Skin | Closed | Has a defect |
Lumen | None | Presence |
Infection risk | Low | High |
Timing of surgery | Can be delayed | Must be early |