Embryology
- Anterior neuropore closes at gestation day 24.
- Caudal neuropore closes at day 26.
Numbers
- Incidence of meningocele or myelomeningocele (MM) is 1–2/1000 live births (0.1– 0.2%).
- Comprised of 98% of open spinal dysraphism
- Risk increases
- Previous birth with MM
- 2–3%: one previous birth with MM
- 6–8%: two previous birth .
- MM in close relatives (e.g. siblings) have given birth to MM children,
- especially when on the mother’s side of the family.
- Risk reduce with folate supplements
- Incidence may increase in times of war, famine or economic disasters, but it may be gradually declining overall.
- myelomeningocele is ~10 to 20 times more common than meningiocele
Aetiology
- Genetic
- non-Mendelian genetics, and is probably multifactorial.
- Environmental
- Prenatal folate (in the form of folic acid) lowers the incidence of MM
- It is recommended that women planning on conceiving start taking folate a few months before conception
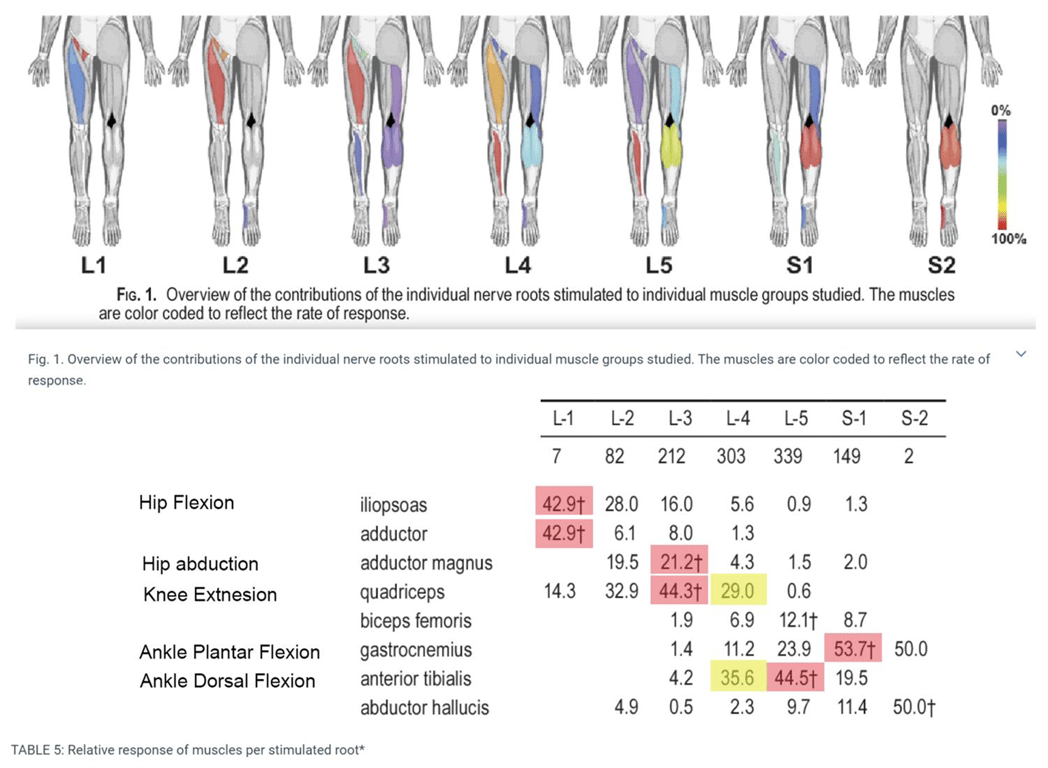
Clinical features at various levels of MM lesion
Paralysis below | Findings | Explanation from moore and dally anatomy text |
T12 | complete paralysis of all muscles in LEs | |
L1 (L2 and below not working) | Weak to moderate hip flexion Palpable contraction in sartorius | Part of iliopsoas working No idea why |
L2 | Strong hip flexion Moderate hip adduction | L2 mains sti for Hip flex (iliopsoas) Some parts of adductor f(x) (Magnus, longus, brevis) |
L3 | Normal hip adduction Almost normal knee extension | L3 is the main stimulation for hip adduction L3 is the main stimulation for knee extension |
L4 | Normal hip adduct Normal Knee ext Normal foot Dorsiflexion/inversion Some hip abduction in flexion | As above As above L4 main supply for Tib Ant No idea why |
L5 | Normal hip adduction, flexion & lateral rotation Moderate Hip abduction Normal knee extension Moderate knee flexion Normal foot dorsiflexion Hip extension absent Produces dorsiflexed foot and flexed thigh | As above L5 dominant Glut medius, Glut mini, Ten fas Lata As above L5 and S1 is co-dominant for semitend/semimemb As above S1 dominant Glut max |
S1 | Normal hip flexion & abduction/adduction, Moderate hip extension and lateral rotation; Normal knee flex & inver/eversion of foot; Moderate plantarflexion of foot; Moderate toes (all) extension Flexion only of terminal phalanx of great toe; Normal medial & lateral hip rotation; Complete paralysis of foot intrinsic (except abductor and flexor hallucis brevis); Produces clawing of toes and flattening of sole of foot | As above As above, lat rotate biceps femoris (L5-S2) As above Codominant S1/S2: gastroc/soleus/plantaris Codominat L5/S1: EDL/EHL/EDB/EHB--> ? X normal S2/3 for all FHL/FHB no f(x), FDB/FDL no f(x)-->?Xnormal As above No idea why Abductor and FHB area all S2/3 innervated |
S2 | difficult to detect abnormality clinically; with growth this produces clawing of the toes due to weakness of intrinsic muscles of sole of foot (innervated by S3) |
Prenatal diagnosis
- See Prenatal detection of neural tube defects.
Management
Intrauterine closure of MM defect
- Controversial.
- Pros
- reduce incidence of Chiari II defect, but it has not been determined if this is clinically significant.
- Argued whether this reduces incidence of hydrocephalus.
- Does not improve distal neurologic function.
Assessment and management of lesion
- measure size of defect
- assess whether lesion is ruptured or unruptured
- ruptured:
- Abx (e.g. nafcillin and gentamicin; D/C 6 hrs after MM closure, or continue if shunt anticipated in next 5 or 6 days)
- unruptured:
- no antibiotics necessary
- Some units give prophylactic abx
- cover lesion with telfa + sponges soaked in normal saline (form a sterile gauze ring around the lesion if it is cystic and protruding) to prevent desiccation
- Prone position, patient on stomach (keeps pressure off lesion)
Neurological assessment and management
- items related to spinal lesion
- watch for spontaneous movement of the LEs
- Good spontaneous movement = better functional outcome
- Assess lowest level of neurologic function by checking response of LEs to painful stimulus:
- 50% have a clear demarcation between normal and abnormal levels,
- 50% show some mixture of normal, reflex, and autonomous activity (arising from uninhibited anterior horn motor neurons) – differentiating reflex movement from voluntary may be difficult.
- Voluntary movement is not stereotyped with repetitive stimulus
- Reflex movement usually only persists as long as the noxious stimulus is applied
- Items related to the commonly associated Chiari type 2 malformation:
- Measure OFC:
- Monitoring risk of developing hydrocephalus
- Use OFC graphs,
- look for abnormal rate of growth (> 1cm/day)
- Head U/S within ≈ 24 hrs
- Check for inspiratory stridor, apneic episodes
MDT assessment
- Neonatologist:
- assess for other abnormalities, especially those that stop surgery (e.g. pulmonary immaturity).
- Average incidence of 2–2.5 additional anomalies in MM patients
- Urology
- Regular urinary catheterizations
- Spine:
- Orthopaedic:
- AP & lat spine films: assess scoliosis (baseline)
- Hip or knee deformities
- Due to neurological lesions
Surgical management
Timing of MM closure
Prenatal surgery
- MOMS
- Within 26 weeks
- Early closure
- Lower infection rate
- After ≈ 36 hrs the back lesion is colonized and there is increased risk of postoperative infection
- Latest closure is 72 hrs
- Not associated with improvement of neurologic function,
- Within 24 hrs whether or not membrane is intact
Simultaneous MM defect closure + VP shunting
- If no hydrocephalus: wait 3 days after MM repair before shunting.
- If clinically overt HCP at birth (ventriculomegaly with enlarged OFC and/or symptoms),
- MM repair and shunting may be performed in the same sitting without increased incidence of infection, and with shorter hospitalization.
- Reduces the risk of MM repair breakdown previously seen during the interval before shunting.
- Technique:
- Prone → head turned to right (to expose the right occiput) → right knee and thigh flexed to expose right flank
- Consider using left flank to prevent confusion with appendectomy scar later in life
Surgical technique of myelomeningocele repair
Outcome
Without treatment | With treatment |
14-30% survive infancy | 85% survive |
70% normal IQ | 80% normal IQ |
50% ambulatory | 3-10% urinary continence (most remain dry with intermittent self-catheterization) |
Without any treatment
- Only 14–30% of MM infants survive infancy;
- these usually represent the least severely involved;
- 70% will have normal IQ’s.
- 50% are ambulatory.
With modern treatment
- 85% of MM infants survive.
- Early mortality
- Due to are complications from Chiari 2 (respiratory arrest, aspiration…),
- Late mortality
- Due to shunt malfunction.
- 80% will have normal IQ.
- Mental retardation is most closely linked to shunt infection.
- 40–85% are ambulatory with bracing
- Most choose to use wheelchairs for ease.
- 3–10% have normal urinary continence,
- but most may be able to remain dry with intermittent catheterization
Complications of myelomeningocele
Hydrocephalus:
- Develops in 65–85% of patients with MM
- 5–10% of MM patients have clinically overt HCP at birth.
- >80% of MM patients who will develop HCP do so before age 6 mos.
- Most MM patients + HCP will have an associated Chiari type 2 malformation
- Closure of the MM defect may convert a latent HCP to active HCP by eliminating a route of egress of CSF.
- Monitor
- Serial head measurements
- USS
- Do not use Ventricular index to monitor
MOMS criteria for shunt placement
- At least two of the following: OR
- An increase in the greatest occipital-frontal circumference adjusted for gestational age defined as crossing percentiles.
- Patients who cross centiles and subsequently plateau do not meet this criteria
- A bulging fontanelle (defined as above the bone assessed when the baby is in an upright position and not crying) or split sutures or sunsetting sign (eyes appear to look downward with the sclera prominent over the iris)
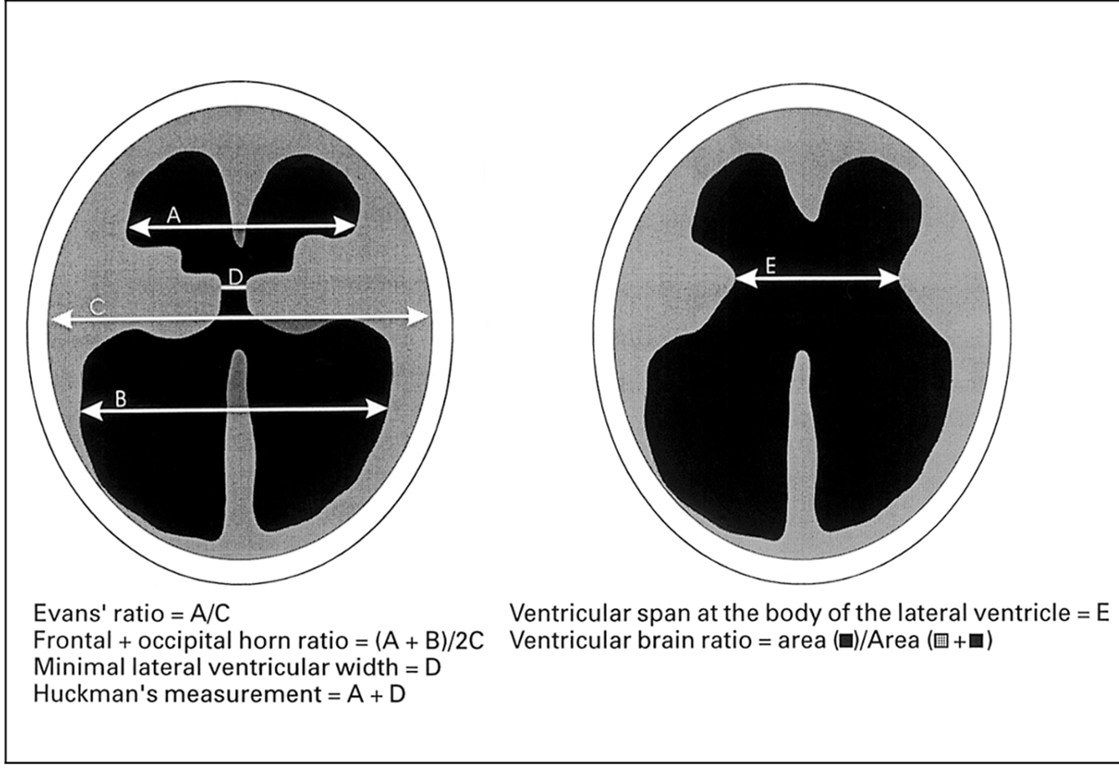
- Increasing hydrocephalus on consecutive imaging studies determined by increase in ratio of biventricular diameter to biparietal diameter according to the method of O’Hayon et al.
- Since the occipital horns are often disproportionately enlarged in paediatric patients, we developed a ratio which averaged the frontal and occipital horn width divided by the interparietal diameter (akin to Evans’ ratio) referred to as the frontal and occipital horn ratio.
- =(A+B)/2C
- Head circumference > 95th percentile for gestational age
- Presence of marked syringomyelia (syrinx with expansion of spinal cord) with ventriculomegaly (undefined).
- Ventriculomegaly (undefined) and symptoms of Chiari malformation (stridor, swallowing difficulties, apnea, bradycardia)
- Persistent cerebrospinal fluid leakage from the myelomeningocele wound or bulging at the repair site
- Post shunting
- may mimic ≈ anything listed below.
- There is no change in ventricular size in significant proportion of those subsequently found to have shunt malfunction.
- In a few cases, a shunt tap may provide useful information.
- ALWAYS RULE OUT SHUNT MALFUNCTION when an MM patient deteriorates
Syringomyelia (and/or syringobulbia)
- Seen in
- Shunt malfunction or
- Shunt revision often diminishes or reverses the asymptomatic hydromyelia, as may cord untethering and these should be considered before other treatment.
- untreated hydrocephalus
- but is often present in asymptomatic individuals.
- Present as
- Rapidly progressive scoliosis
- Weakness of the upper extremities
- Spasticity
- An ascending motor loss in the lower extremities
- It is rare in the newborn, and usually develops with the first shunt malfunction.
- Tx hydromyelia
- VP Shunt
- Detethering
- Fenestration and shunting (either to the subarachnoid space or peritoneal cavity),
- If the above two options do not work can try
- but these approaches can paradoxically increase the defect, cause tethering, or create an imbalance with the ventricular shunt.
Latex allergy
- 73% of MM patients are allergic
- Protein in latex
- Milky sap from the rubber tree
- Due to early and frequent exposure to latex products during medical care for these patients,
- Latex-free surgery on these infants may reduce the risk of the development of latex allergy.
Tethered cord syndrome
- 70% of MM patients have a radiographic tethered cord
- Only a minority are symptomatic.
- Unfortunately no good test to check for symptomatic retethering (SSEPs may deteriorate, myelography may help):
- Scoliosis: early untethering of cord may improve scoliosis;
- Symptomatic tethering may manifest as delayed neurological deterioration
- Untethering will be easier if the exposed neural tissue was closed into a tube during the primary closure.
Medullary compression at foramen magnum (Chiari II malformation)
- The brainstem or spinal cord is compressed within the spinal canal, causing progressive neurological dysfunction, including bulbar palsy, apneic episodes.
- When decompression is indicated a variety of approaches are used, including cervical bone-only decompression, dural opening (with or without a graft to increase the size of the canal), resection of the cerebellar tonsils, stent placement into the 4th ventricle, or a combination.
Dermoid tumour at MM site:
- Incidence ≈ 16%
Impaired cognitive development
- Due to
- Chiari II malformation
- Hydrocephalus
Urinary tract complications.
- Nearly all patients with myelomeningocele have bladder dysfunction (neurogenic bladder),
- They can develop progressive deterioration of the upper urinary tract and chronic renal disease.
- Close attention to urinary tract function is also important because changes in bladder function may be the only indication of a change in neurologic function and should prompt an evaluation for
- shunt malfunction
- hydrocephalus
- tethered cord.
- Management
- clean intermittent catheterization,
- antibiotic prophylaxis
- anticholinergic medication to reduce vesicoureteral reflux.
Bowel management.
- Almost all myelomeningocele have abnormal innervation of the bowel and anus → leading to dysmotility
- poor sphincter control → fecal incontinence.
- Decreased bowel motility → constipation and fecal impaction → elevation in intra-abdominal pressure → shunt malfunction.
- Tx
- Oral laxatives, suppositories, and enemas, bowel program (gastrocolic reflex), transanal irrigation or surgical antegrade continence enema.
Orthopaedic problems.
- Aim
- Correcting deformities
- Maintaining posture
- Promoting ambulation to maximize function and independence,
- Myelomeningocele pt often have congenital skeletal deformities involving the feet, knees, hips, and spine.
- Scoliosis occurs in most children with lesions above the second lumbar vertebra (L2).
- New or rapidly progressive scoliosis in an individual with myelomeningocele may be caused by a reversible neurologic complication such as
- Shunt malfunction
- Tethered cord
- Hydromyelia
Other
- Use of growth hormone to increase stature is controversial
- Pressure ulcers