Prenatal detection of neural tube defects
Serum alpha-fetoprotein (AFP)
- High maternal serum AFP (≥2 multiples of the median for the appropriate week of gestation) between 15 and 20 weeks gestation carries a relative risk of 224 for neural tube defects
- An abnormal value (high or low)
- Associated with 34% of all major congenital defects.
- Sensitivity of maternal serum AFP
- Spina bifida: 91% (10 of 11 cases)
- Does not detect closed lumbosacral spine defects, accounting for ≈ 20% of spina bifida patients
- Anencephaly: 100% for 9 cases
- Since maternal serum AFP rises during normal pregnancy, an overestimate of gestational age may cause an elevated AFP to be interpreted as normal, and an underestimate may cause a normal level to be interpreted as elevated.
- When the serum AFP is positive, repeat the serum AFP because repeat testing will be negative in many cases, and such findings are not associated with an increased frequency of false-negative NTD diagnoses.
Ultrasound
- Will detect 90–95% of cases of spina bifida
- before 12th post menstrual week Looking for
- Irregularities of the bony spine or a bulging within the posterior contour of the fetal back.
- After the 12th postmenstrual week, looking for
- Chiari II malformation signs
- lemon sign
- A concave shape of the frontal calvarium.
- banana sign
- Posterior convexity of the cerebellum in the presence of spina bifida.
- Ventriculomegaly
- Microcephaly
- Obliteration of the cisterna magnum.
- In cases of elevated AFP, it can help differentiate NTDs from non-neurologic causes of elevated AFP (e.g. omphalocele), and can help to more accurately estimate gestational age.
Amniocentesis
- For pregnancies subsequent to an MM, if prenatal ultrasound does not show spinal dysraphism, then amniocentesis is recommended (even if abortion is not considered, it may allow for optimal postpartum care if MM is diagnosed).
- Amniotic fluid AFP levels are elevated with open neural tube defects, with a peak between weeks 13 and 15 of pregnancy.
- Amniocentesis also carries a ≈ 6% risk of fetal loss in this population.
Risk factors
- After one child with spinal dysraphism is born, the risk will increase to 5% for subsequent childbirth.
- Lack of prenatal folic acid:
- Confirm that vitamin B12 levels are normal
- Folate antagonists
- e.g. carbamazepine
- doubles the incidence of MM
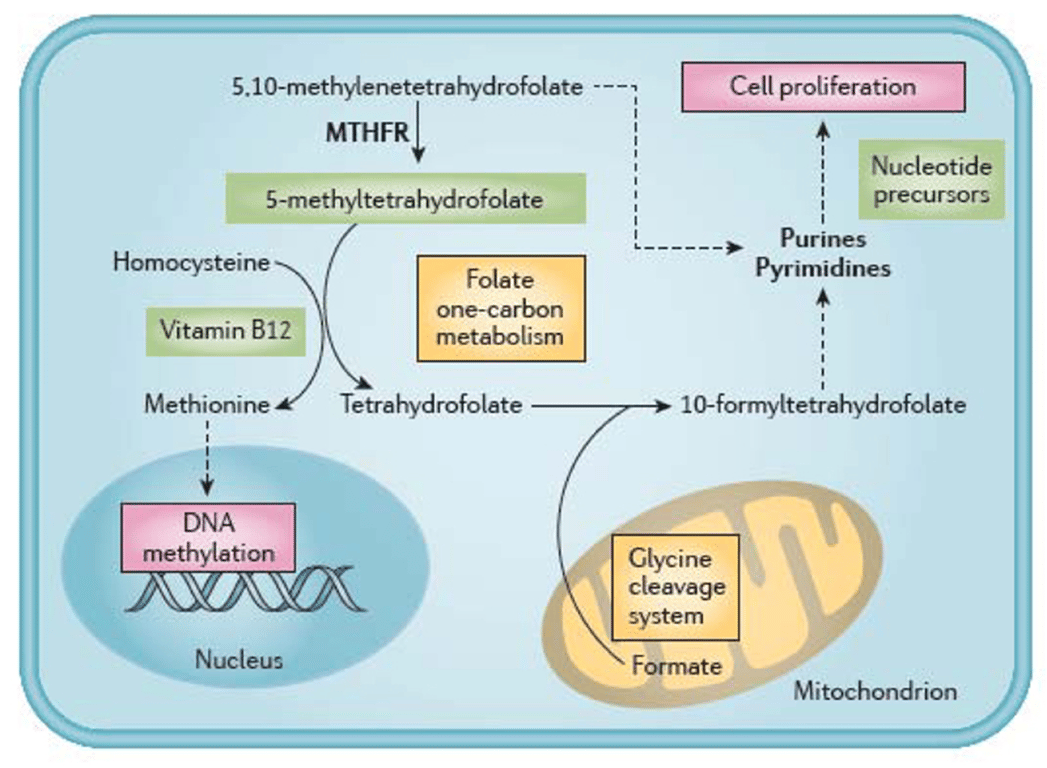
- Mothers with 5, 10-methylenetetrahydrofolate reductase (MTHFR) gene polymorphism
- The common variant, C677 T, substitutes an alanine residue for valine at position 222 in the folate dependent MTHFR enzyme → decreased enzyme activity → reduced levels of tissue folate, and increased levels of homocysteine in the plasma.
- This polymorphism may be
- Homozygous (TT genotype)
- Present in ≈ 10% of population
- Heterozygous (CT genotype);
- Present in ≈ 38% of the population
- The effects with the TT genotype are more pronounced than with the heterozygous CT form,
- Increased risk of
- Neural tube defects
- Cardiovascular disease
- Valproic acid (Depakene®) during pregnancy is associated with a 1–2% risk of NTD
- Maternal heat exposure
- Eg: hot-tubs, saunas or fever (but not electric blankets)
- in the first trimester was associated with an increased risk of NTDs
- Obesity (before and during pregnancy) increases the risk of NTD
- Maternal cocaine abuse may increase the risk of
- Microcephaly
- disorders of neuronal migration
- neuronal differentiation
- myelination
Prevention of neural tube defects
Folic acid
- Difference between folate and folic acid
Folate | Folic Acid |
Naturally occurring form of vitamin B9 | Supplemental form of vitamin B9 |
Found in foods like beans, peas, lentils, leafy green vegetables | Found in many supplements and fortified foods like breads and cereals |
May be challenging to meet daily recommendations, especially for pregnancy, through food alone | Often used in prenatal vitamins as the methylated form L-5-methyltetrahydrofolate, which is more easily utilized by the body |
- Similarities between folate and folic acid
- Help reduce the odds of neural tube defects
- Support healthy development of the nervous system
- Play a role in DNA synthesis.
- Support healthy methylation in the body
- Cochrane: Folic acid supplements before conception and in early pregnancy (up to 12 weeks) for the prevention of birth defects
- Dose
- early administration of folic acid (conceive to 12 weeks)
- 0.4 mg/d if no history of neural tube defects
- 4mg/d in a carrier or with previous child with NTD
- Associated with a 71% reduction in recurrence of NTD
- Daily Recommendation
- Adults/preconception: At least 400 micrograms
- Pregnant women: At least 600 micrograms
- Reduce the occurrence of
- Neural tube defects (NTDs).
- Spina bifida
- Anencephaly
- Other birth defects (possibly)
- cleft lip, with or without cleft palate,
- congenital cardiovascular defects.
- Recommendation
- Supplementation with folic acid is internationally recommended to women from the moment they are trying to conceive until 12 weeks of pregnancy.
- WHO:
- Women of reproductive age take intermittent (weekly) iron and folic acid supplements, especially in populations where the prevalence of anaemia is above 20%.
- Recently, 5-methyl-tetrahydrofolate (5-MTHF) has been proposed as an alternative to folic acid supplementation.
- This is because most dietary folate and folic acid are metabolised to 5-MTHF. Some women have gene characteristics which reduce folate concentration in blood.
- Cost-effectiveness - Holdinott 2018
- National mandatory food fortification promotes health equity & highly cost-effective
- Estimated cost per death averted = US$ 950
- Estimated cost per disability adjusted life year (DALY) averted = US$ 15
- Cost-effectiveness of FA fortification is similar to other life-saving interventions (rotavirus vaccines & bed nets)
- Recent estimates suggest 18–32:1 return on investment using folic acid fortification