General
- Aka: Child abuse, Non accidental injury, shaken baby syndrome, nonacccidental head injury, abusive head trauma
Definition
- Inflicted cranial and spinal injuries resulting from blunt force trauma, shaking or a combination of forces
Numbers
- Leading cause of death in child abuse
- This is the most serious form of physical abuse out of all the child abuses
- Mortality: 30%
- Morbidity: 50% (of survivors)
- At least 10% of children <10 yrs of age that are brought to E/R with alleged accidents are victims of child abuse.
- The incidence of accidental head trauma of significant consequence below age 3 is low, as this is the age group in which battering is highest.
- Majority of patients <1 yrs old
Risk factor
- Baby factor
- Prematurity
- Twin male
- Physical handicaps
- Stepchild
- Parents factor
- Young parents
- Dec. Socioeconomic status
- 1/3 of parents are under influence of drug or alcohol when abusing the baby
Mechanism
- Direct impact injury
- Direct blow to head or head impact onto an object
- Skull fractures and injury to underlying brain
- Shaking injury: Violent "to and fro" of head
- Diffusely distributed subdural haematoma
- Cortical contusion
- Axonal injury
- Parenchymal lacerations
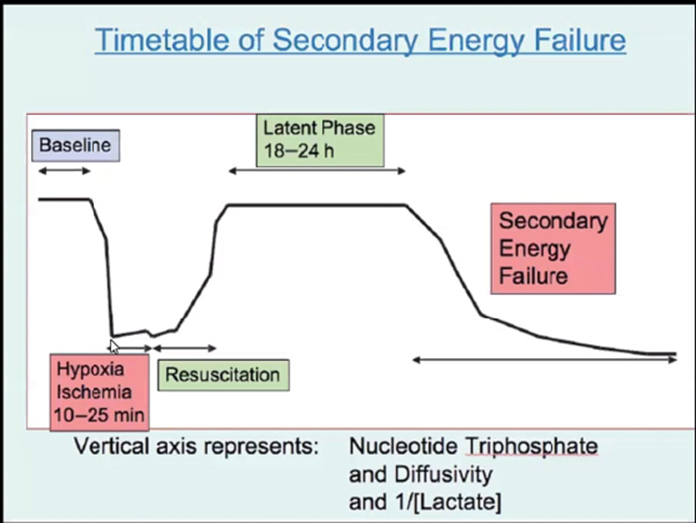
- Hypoxic ischaemic injury
- Initial cardiorespiratory arrest
- Seizures through excitotoxic process
- Glutamate
- Secondary energy failure
Types of injuries
- Scalp injuries
- Skull fractures
- Intracranial haemorrhage
- Significantly associated with AHT (>50% cases)
- Location
- Convexity
- Interhemispheric
- Post fossa
- Secondary to tearing of bridging veins
- Timing
- Acute (hrs -days)
- 60% homogenously hyper dense
- 40% mixed hyper, hypodense
- Torn arachnoid with CSF accumulation
- Active bleeding (swirl sign)
- Clot retraction
- Rare: isodense aSDH
- Anaemia
- Coagulopathy
- Subacute (7-22 days)
- Rapid, variable changes
- Density
- Iso: 40%
- Hypo: 50%
- Hyper: 10%
- Neomembranes develop by 2-3 wks
- Mix density SDH:
- IS NOT acute on chronic haemorrhage
- Rather it is (can derive from a single traumatic event)
- Hyper acute + acute blood
- Acute haemorrhage alone
- Haematohygroma (acute HGE + CSF from arachnoid tear)
- Combination of new and old haemorrhage
- Chronic (>22 days)
- Features related to age and rebleed from neomembranes
- Isodense (87%)
- Hypo (13%)
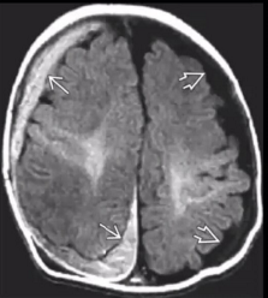
- Subdural hygromas
- CSF like density/intensity
- Part of evolution of SDH
- May develop acutely
- Neomembranes
- Begin to form within SDH by 2-3 wks and mature by 4-5 wks
- MRI >>>> CT: Membranes enhances
- Contains fragile capillaries --> risk of rebleeds
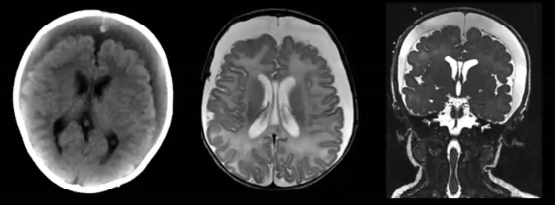
SDH
Density evolution of haemorrhage on CT
Stage | Appearance | Estimate of age |
Hyperacute | Isodense | < 3 hours |
Acute | Hyperdense | Few hours → 7-10 days |
Subacute | Isodense | 2-3 weeks |
Chronic | Hypodense | > 3 weeks |
flowchart LR A["HEAD TRAUMA"] == BV injury ==> B["acute SDH"] B == "rapid resorption of subdural blood<br>cleaved dura-arachnoid-interface under decreased ICP<br>CSF and CSF-like liquid effuses from the environment" ==> C["Subdural hygroma"] B -. "approx. 1/3" .-> E["complete resolution / resorption"] C -. majority .-> E C == expansion under decreased ICP<br>formation of neomembranes including new vessels (neovascularization)<br>microhemorrhages ==> D["chronic SDH"] B --> D A -.-> C style A stroke:#D50000, fill:#D50000, color:#FFFFFF style B stroke:#D50000, fill:#D50000, color:#FFFFFF style C stroke:#D50000, fill:#D50000, color:#FFFFFF style E stroke:#00C853, fill:#00C853, color:#FFFFFF style D stroke:#D50000, fill:#D50000, color:#FFFFFF linkStyle 0 stroke:#D50000,fill:none linkStyle 1 stroke:#D50000,fill:none linkStyle 4 stroke:#D50000
EDH
SAH
IVH
IPH
- Cerebral contusions
- Shear injuries
- Ischaemic brain injuries
Clinical features
- Highly variable
- Irritability
- Vomiting
- Apnea
- Seizure
- Obtundation
- Vague and variable hx
- "Killer couch" -FAKE
- Injuries attributed to infant rolling off couch onto floor
- Chadwick 2008: Annual risk of death resulting from short falls among young children: less than 1 in 1 million
- There are no findings that are pathognomonic for child abuse. Factors which raise the index of suspicion include:
- Retinal haemorrhage
- Bilateral chronic subdural hematomas in a child< 2 yrs of age
- Skull fractures that are multiple or those that associated with intracranial injury
- Significant neurological injury with minimal signs of external trauma
- Multiple injuries of different ages in multiple locations
- Bruising on the buccal surface of the lips is a high risk sign of NAI
Evaluation
- Skull fx on x-ray or clinical signs of intracranial injury → CT →
- MRI
- to assess extent of injury and to confirm injury
- Also to be done in patients with abuse even with no evidence of intracranial injury
- X-ray skeletal survey
- Bone scintigraphy
- U/S
- CT
- Test of choice
- Pros
- Quick
- Avoid sedation
- Easily accessible
- Accurately detects subdural haemorrhage and fx
- Cons
- Exposure of brain to ionizing radiation
- Babies more vulnerable, has longer life span to develop cancer
- Protocol
- Age adjusted settings → reduce radiation
- Soft tissue reconstruction at 3mm, bone reconstructions at 0.6mm
- MPR
- Improves intracranial haemorrhage and fracture detection
- 3D
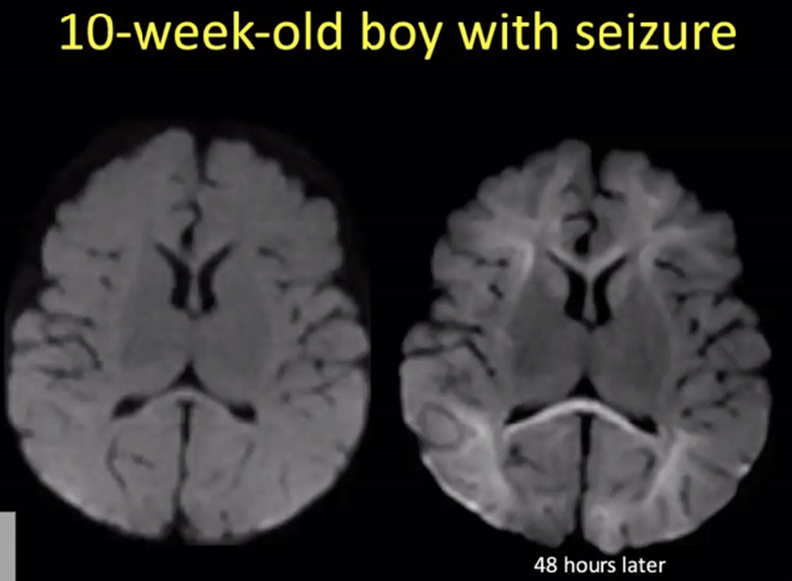
- MRI
- Performed 48-72 hrs after presentation
- Pros
- Avoid radiation
- Cons
- Requires child to motionless for mins to hrs
- May require sedation
- Most centres don't have the resource to do this
- Protocol
- DWI
- Sag T1 3d + MPR
- T2 axial +Coronal
- Sag Flair 3D + MPR
- SWI
- MR venogram with contrast
- Contrast enhanced T1 3D + MPR
- Fast MRI
- Featurs
- Abbreviated exam
- Motion tolerant sequences
- Avoid sedation
- Eliminates radiation
- Use fq in shunted hydrocephalus
- Composed of
- Axial and Coronal T 2 SSH
- Axial Tl SSH TFE
- Axial FLAIR SSH
- Axial gradient echo
- Axial DWI
- Total scan time 6 min
- Of the 223 pts, CT identified TBI in 50% skull fractures, subdural hematomas, SAH
- Fast MRI:
- Sensitivity 93%, Specificity 96%
- 8 cases of TBI visible on CT, missed by Fast MRI
- 5 cases of TBI visible on Fast MRI, missed by CT
- 4 cases where CT raised concern for hypodense SDH but fast MRI concluded enlarged subarachnoid spaces
Prognosis
- Acquired microcephaly (93%)
- Early post-traumatic seizures (79%)
- Late post-traumatic epilepsy (>20%)
- Poor visual outcome (20-65%)
- Outcome
Condition | Percentage Range |
Death | 20-25% |
Spastic hemiplegia or quadriplegia | 15-64% |
Intractable epilepsy | 11-32% |
Microcephaly with cortico-subcortical atrophy | 61-100% |
Visual impairment | 18-48% |
Language disorders | 37-64% |
Agitation, aggression, tantrums, attention deficits, memory deficits, inhibition or initiation deficits | 23-59% |
Differentials for NAI
- Coagulopathy
- Leukaemia
- Haemangiomas
- Osteogenesis Imperfecta
- Glutaric Aciduria Type 1 — SDH and macrocephaly
Shaken baby syndrome
- Brain injury due to vigorous shaking of child
- Vigorous shaking --> whiplash-like angular acceleration-decelerations of the head (the infant head is relatively large in proportion to the body, and the neck muscles are comparatively weak) --> brain injury.
- Some researchers believe that shaking alone may be inadequate to produce the severe injuries seen, and that impact is often also involved.
- Clinical features
- Retinal haemorrhages
- Extradural haematoma
- External trauma required
- Subdural hematomas (bilateral in 80%)
- No external trauma required
- Subarachnoid haemorrhage (SAH).
- Few or no external signs of trauma
- including cases with impact, although findings may be apparent at autopsy.
- Finger marks on the chest,
- Multiple rib fractures and/or pulmonary compression ± parenchymal lung haemorrhage.
- Deaths in these cases are almost all due to uncontrollable intracranial hypertension.
- There may also be injury to the cervicomedullary junction.
Retinal haemorrhage (RH)
- the presence of RH is pathognomonic of NAI.
- RH may also occur in the absence of any evidence of child abuse.
- 16/26 battered children < 3 yrs of age had RH on fundoscopy, whereas,
- 1/32 non-battered traumatized children with head injury had RH
- The single false positive: traumatic parturition, where the incidence of RH is 15–30%.
- Differential diagnosis of aetiologies of retinal haemorrhage:
- Child abuse
- benign subdural effusion in infants
- acute high altitude sickness
- acute increase in ICP:
- e.g. with a severe seizure
- Purtscher’s retinopathy:
- loss of vision following major trauma (chest crush injuries, airbag deployment…), pancreatitis, childbirth or renal failure, among others.
- Posterior pole ischemia with cotton-wool exudates and haemorrhages around the optic disc due to microemboli of possibly fat, air, fibrin clots, complement-mediated aggregates, or platelet clumps.
- No known treatment
Skull fractures in child abuse
- Parietal bone was the most common site of fracture in both groups (≈ 90%)
- Depression of skull fractures was frequently missed clinically due to overlying hematoma
- Clinical features in patients with skull fractures (retinal haemorrhage) did not reliably differentiate child abuse from trauma
- 3 characteristics more frequently seen after child abuse than after other trauma:
- Multiple fractures
- Bilateral fractures
- Fractures that cross sutures
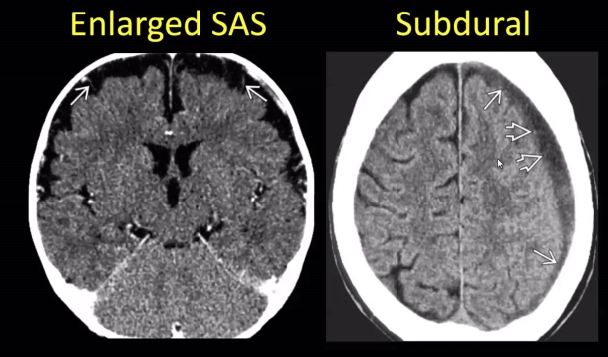
Benign enlargement of subarachnoid spaces vs subdural haematoma
Controversies with child abuse that are not true
- Venous thrombosis causing SDH from back pressure
- No evidence for this mechanism in autopsy or case reports
- Basically back pressure is not high enough to cause SDH
- Hypoxic ischaemic injury causing SDH in paeds
- False
- Sustained Valsalva from coughing or choking causes SDH or retinal haemorrhage
- Raised Intrathoracic pressure --> inc. venous pressure --> venous rupture of
- Fake
- SDH due to rebleeding secondary to birth related SDH
- Birth related trauma
- Scalp soft tissue
- Skull
- Extracerebral/intracranial haemorrhage
- Brain parenchymal injury (haemorrhage/contusion)
- Birth related SDH is present in 50%
- Due to vaginal delivery, spontaneous and assisted
- Associated with longer first and second stages of labour
- Increase prolonged propulsive and compressive forces, increased moulding and overlapping of sutures
- Vast majority resolve by 4 wks if not by 3 months all resolved
- No evidence for this mechanism as an explanation for SDH
- Enlarged subarachnoid spaces
- Idiopathic enlargement at 1 yr of life
- Subdurals occur in 5.3% of cases of enlarged subarachnoid spaces
- Mech (unknown)
- Immature CSF drainage
- Typically bifrontal +/- ventriculomegaly
- No neurological sequelae after resolution (2 yrs to resolve)
- However if there is an increase in OFC above 95% think of abuse
- If concerned get an MRI
flowchart LR C["Timely presentation and consistent history"] --> D["No injury identified"] & F["Injury identified: manage<br>injury<br>discuss with senior"] D --> E["Discharge patient"] F --> G["Discharge"] & H["Any concern identified"] H --> I["Admit under shared care<br>appropriate specialty/child<br>protection team<br>Consider the need for: CTH,<br>Skeletal survey, NAI bloods<br>(See below), Ophthalmology<br>review,<br>Contact Stand-by Social<br>Work and/or Police to<br>ensure safety of siblings"] A["Presentation to ED<br>with physical injury<br>(Child < 1 year of age)"] --> n1["Concern about hx<br>Discuss with senior"] & C n1 --> n2["Senior has no concern"] n2 --> n3["Discharge"] n1 --> H
- Senior: Child protection team and consultant
NAI bloods
- Intrinsic Coagulation factors VIII, IX, XI, XII
- Urine Organic Acids
- Bone Profile
- Vitamin C
- PTH
- Vit D
- CRP
- LFT
- U/E
- Factor VIII activity
- Coag screen
- FBC