General information
- Aka:
- Traumatic leptomeningeal cysts
- Growing skull fractures
- Not to be confused with arachnoid cysts (AKA leptomeningeal cysts, which are not posttraumatic).
Definition
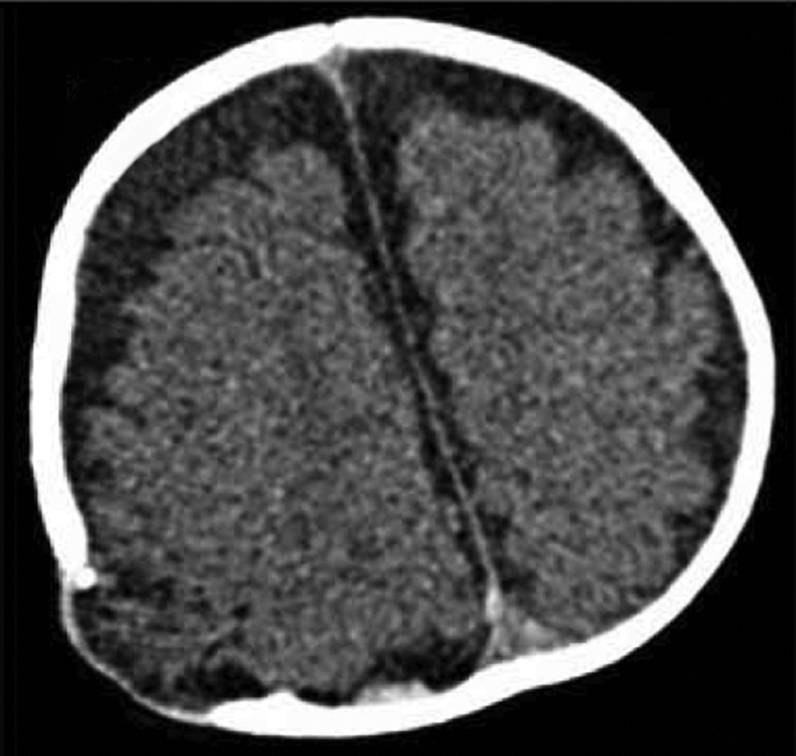
- A fracture line that widens with time.
Numbers
- are very rare, occurring in 0.05–0.6% of skull fractures.
- Mean age at injury: <1 year:
- >90% occur < 2 years old#
- Formation may require the presence of a rapidly growing brain
- Rare adult cases have been described
Pathology
- Prerequistes
- widely separated fracture AND
- a dural tear AND
- brain injury at the time of the fracture with displacement of leptomeninges and possibly brain through the dural defect AND
- Subsequent enlargement of the fracture to form a cranial defect
- Mech
- Dural tear → dural pulsation widens the dural tear → dural pulsation causes the dura to hernia into the fracture and widens the fracture.
- Can also occur in
- Osteogenesis imperfecta
- NF1 bone dysplasia
- Pseudogrowing fracture:
- Some children may develop a skull fracture that seems to grow during the initial few weeks that is not accompanied by a subgaleal mass, and that heals spontaneously within several months.
Presentation
- PTLMCs rarely occur>6 mos out from the injury.
- Mainly asymptomatic
- Skull defects
- Mass effect
- Scalp mass (usually subgaleal)
- Headache
- persistent or progressive neurological deficits
- Seizures
Evaluation
- Radiographic findings:
- progressive widening of fracture and scalloping (or saucering) of edges.
- Screening for development of PTLMC
- If early growth of a fracture line with no subgaleal mass is noted, repeat skull films in 1–2 months before operating (to rule out pseudogrowing fracture).
- In young patients with separated skull fractures (the width of the initial fracture is rarely mentioned), consider obtaining follow-up skull film 6–12 mos post-trauma.
- <1 yr old post linear skull fracture should be followed up (at 1 year) to exclude the development of a growing skull fracture.
Management
- Treatment of true PTLMC is surgical,
- Technique
- Surgical resection of the leptomeningeal cyst and degenerated brain tissue
- Since the dural defect is usually larger than the bony defect, it may be advantageous to perform a craniotomy around the fracture site, repair the dural defect, and replace the bone.
- Water-tight repair of the dural defect (either primary or with duraplasty)
- Closure of the bony skull defect.
- In younger children (especially infants) it is technically difficult to split the skull bone to make enough materials for closure of the defect. So need cranioplasty
- If PTLMC is diagnosed in the early stages, especially the prephase of GSF, these problems can be easily resolved.
- Pseudogrowing fractures should be followed with Xrays and operated only if expansion persists beyond several months or if a subgaleal mass is present.