General
- A rare disorder.
Aetiology
- With trauma
- especially with violent hyperflexion or hyperextension of the neck after RTA
- Predilection for pediatrics,
- possibly due to the higher ratio of head to body weight, flatter occipital condyles, and increased ligamentous laxity in children.
- Without trauma
- more likely in adults e.g.
- pituitary apoplexy
- Anticoagulation
- subarachnoid hemorrhage
Pathology
- Blood can be epidural (anterior to the tectorial membrane or subdural (posterior to tectorial membrane) or a combination, and may originate from fracture or ligamentous disruption.
- May be associated with:
- Atlantooccipital dislocation
- occipital condyle fracture
- disruption of the apical odontoid ligament
- fracture of the clivus
- odontoid fracture
Presentation
- Neurologic findings may be due to stretching, compression, or contusion of adjacent brain parenchyma or nerves.
- Cranial nerve presentation:
- abducens (VI):
- the most commonly involved cranial nerve.
- May be unilateral or bilateral
- optic (II)
- oculomotor (III)
- trigeminal (V)
- facial (VII)
- glossopharyngeal (IX)
- hypoglossal (XII)
- spinal accessory nerve (XI)
- Other presentations include:
- hemiparesis
- quadriparesis
- Hydrocephalus
- occipitocervical instability
Imaging
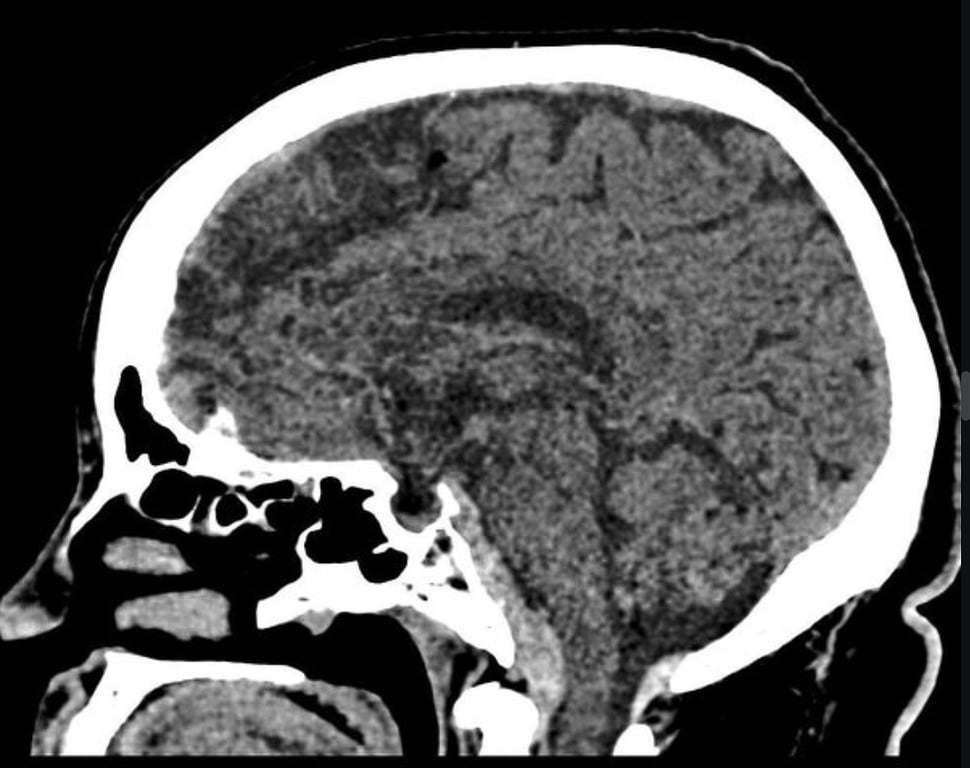
- CT
- coronal reconstructions is useful to look for
- occipital condyle fractures,
- avulsion of the apical ligament,
- assess the atlantooccipital interval
- Surrogate marker for atlantooccipital dislocation
- CTA
- for concurrent blunt cerebrovascular injury
- Indicated
- if stroke is suspected or demonstrated on MRI
- MRI
- Noncontrast MRI
- imaging modality of choice.
- Demonstrates the hematoma (acutely may be best seen on T2WI),
- DWI assesses for stroke,
- STIR images to look for signal changes indicative of ligamentous injury
Management
- Conservative:
- Most are managed
- Usually with a brace (halo/vest, SOMI…).
- Surgery
- Indications
- fusion:
- strong indication:
- ligamentous instability e.g. atlantooccipital dislocation meeting AOD surgical criteria
- soft indication:
- cranial nerve deficits
- evacuation of hematoma:
- indicated on rare occasion for symptomatic brainstem compression
- Ventriculostomy/shunt:
- indicated for hydrocephalus
Outcome
- The hematoma generally resolves in 2–11 weeks.
- Conservative management results in good outcomes with minimal long-term neurologic deficits in the majority of cases.
- Death occurs infrequently, and usually from other causes in patients who are neurologically devastated on admission.