TL fractures
- Mech of injury
- In distraction injuries, the deforming tension force is commonly translated through the relatively weak physeal cartilage of the maturing vertebral body, resulting in a Salter-Harris type I fracture, which typically heals well with appropriate immobilization.
- Paeds pt have less protection from overlying muscles and bony structures (underdeveloped iliac crests/ribs), resulting in higher risk for intra-abdominal and intrathoracic organ injuries compared with their older counterparts.
- In compression injuries, a preponderance of multilevel injuries in children may be attributable to increased flexibility and small vertebral bodies allowing only small surface areas for contact with high forces.
- Immature vertebral bodies are also wedge shaped, thus creating a natural kyphosis and a predisposition to compression fractures.
- Physical examination alone is up to 87% sensitive and 75% specific for detecting thoracolumbar spine fracture.
- Palpation of the entire spine and paraspinous region should also be performed while the patient is log rolled, with any step-offs, crepitus, bruising, or open injuries noted.
- Common associated injuries with TL fractures include
- 42% have concomitant abdominal or thoracic trauma
- Especially common in motor vehicle passengers restrained by a seat belt across the lap, given the flexion of the abdomen and compression of visceral structures.
- Eg
- small bowel injuries,
- pancreatic rupture,
- hemothorax or pneumothorax,
- lung contusion,
- aortic injury.
- > 30% may have associated head injury.
- 11-34% chance of multilevel spine involvement
- 6-7% chance of non-contiguous multilevel fractures.
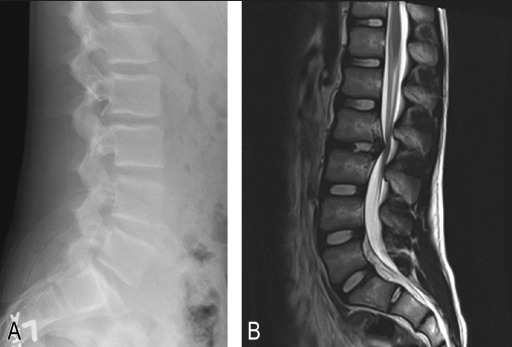
- AP and lateral plain radiographs are often favored for initial imaging, with the addition of MRI for children with neurologic deficits
- CT should not be used as a spine screening examination in children because of the risks associated with ionizing radiation.
- Management of TL fracture
- TLICS Validity was substantially lower in children (80.2% correct in pediatric population versus 95.4% correct in adults), indicating that the TLICS system may not satisfactorily guide the treatment of TL injuries in pediatric patients.
- Use Denis 3-column theory
- placing particular emphasis on the mode of failure to the middle column to stratify fracture types and risk of neurologic injury.
- According to this classification system, the four major types of fractures are compression, burst, flexion-distraction (Chance fractures), and fracture-dislocation injuries.
Compression fractures
- General
- most common in the paediatric spine
- most occurring near the thoracolumbar junction.
- Mech
- Low-energy mechanisms (Falls and sports injuries causing axial loading and flexion of the spine)
- Anterior vertebral body collapse
- Normally totalling < 20% of the body height.
- If > 50% of the anterior height is lost --> MRI ? posterior element disruption
- Often seen in multiple contiguous levels, accentuating the kyphosis seen in paediatric vertebral bodies
- In the absence of posterior element/ligament disruption, there will be no instability of the spine.
- Sagittal vertebral compression fracture
- More common
- heals (with anterior vertebral height restoration) without surgical intervention.
- Coronal/lateral vertebral compression fractures
- are less common
- less likely to show full height restoration
- Fractures of the developing end plate
- result in permanent loss of ability to regain full vertebral height
- Leading to compensatory overgrowth of the adjacent vertebral bodies).
- Tx
- management of choice for multiple compression fractures and TL J(x) compression fractures
- activity modification
- TLSO bracing
- maintained for 6-8 weeks
- Single level compression fractures not close to the thoracolumbar junction
- Bracing optional
- Mainly for pain management
- Outcomes
- excellent healing
- few long-term problems
- Chronic back pain and deformity > 10° are possible.
Burst fracture
- Mech
- axial compression force --> drives the nucleus pulposus into the vertebral body, --> fracture of the anterior and middle columns.
- Commonly at TL junction.
- Retropulsion of the posterior vertebral body and fracture of the posterior elements may lead to
- biomechanical instability,
- neurologic injury,
- dural tear.
- The Denis classification of burst fractures includes
- Type A fractures
- rupture of both end plates.
- Type B fractures
- A single end plate is ruptured in superior end plate
- Type C fractures.
- (inferior end plate)
- Type D
- type A fracture + rotational deformity,
- Type E
- Eccentrically loaded type A, B, or C fracture with lateral flexion deformity.
- Biomechanical instability is suggested by
- Three-column injury
- Focal kyphosis > 20°
- Anterior vertebral collapse > 50%
- Significant retropulsion (> 50%)
- Lamina fracture
- Facet subluxation
- Neurologic injury.
- Imaging
- CT
- assessing the amount of neural compression, posterior element involvement, and osseous retropulsion.
- MRI
- Assessing
- neurologic and ligamentous structures,
- PLC to determine potential stability/instability.
- Management
- Biomechanically stable burst fractures without neurologic compromise
- managed in a hyperextension cast or TLSO brace for 8-12 weeks.
- Due to strength and excellent healing potential of children’s bones, greater ability to remodel/reabsorb retropulsed bone in the spinal canal, reduced risk of late kyphotic deformity and better tolerance of immobilization, conservative management of burst fractures is possible in children.
- Surgical treatment
- Indication
- Partial or progressive neurologic deficit caused by spinal canal compromise treated with decompression
- Prevention of late kyphotic deformity (if > 25° of localized kyphosis present),
- Unstable burst fractures
- Technique
- posterior instrumentation with or without fusion
Distraction injuries
- Aka
- Flexion-distraction injuries
- Chance fractures
- lap belt injuries
- Mech
- distractive force in which the posterior column fails in tension and the anterior column fails in either distraction or compressive flexion.
- Types
- Purely osseous injuries,
- Purely ligamentous/disc injuries
- Combination of bony, disc, and ligamentous injury.
- Associated injuries
- Concomitant visceral and head injuries are common and occur in approximately 40% of paediatric patients with flexion-distraction injuries,
- Management
- extension cast or TLSO immobilization for 8-12 weeks
- Indication
- Purely bony flexion-distraction fractures
- if kyphosis < 20° and the fracture remains well reduced in the cast or brace (standing X-rays).
- Surgery
- Indication
- If acceptable alignment cannot be maintained nonsurgically
- Purely ligamentous injuries
- are less likely to heal than purely bony injuries,
- Very unstable fractures that cannot be managed in a brace
- Fractures with significant kyphosis that cannot be reduced or maintained in a brace
- Fractures associated with neurologic injury or abdominal injury.
- Aim
- Reconstitute a sufficient posterior tension band
- Technique
- Posterior wiring
- in small children
- Posterior instrumentation
- Older children
- Pedicle screw instrumentation is most often extended one or two levels above and below the injury, with posterior compressive force used for anatomic reduction.
- Sometimes anterior fusion is required
- Posterolateral gutter fusion is often performed following instrumentation.
- neural elements decompressed
Vertebral end plate fractures
- Aka
- Apophyseal rim/ring fractures and herniations
- Limbus fracture
- Numbers
- Mech
- Traumatic disruption of the vertebral ring apophysis and disc with extrusion into the spinal canal, analogous to adult intervertebral disc herniation.
- They generally occur in children 10-14 years of age due to the open physes (growth plates) in the vertebral column.
- The injury occurs as a result of a separation of the vertebral apophysis from the spongiosa layer of the vertebral body, with the fracture traversing the hypertrophic zone of the physis.
- The caudal physis is more often involved than the cranial physis (in contrast to congenital limbus vertebra).
- Clinical features
- Same as a herniated disc and include back and leg pain, muscle spasm, and root tension signs
- neurologic signs such as muscle weakness, sensory changes, and absent reflexes may also be present.
- Patients with significant stenosis may describe symptoms consistent with neurogenic claudication.
- Imaging
- May be purely cartilaginous with herniation of the apophysis and disc or osseous with fractures of the cortical and cancellous rim of the vertebral body.
- This type of injury may spontaneously reduce and may not be seen on plain radiographic imaging, although with scrutiny, a small flake of bone may be seen posterior to the vertebral body.
- If apophyseal herniation is suspected, MRI should be obtained to evaluate the location and size of the herniation.
- Management
- In the absence of neurologic deficits, anti-inflammatory medication and 8 weeks of TLSO bracing is usually curative; however, chronic back pain may ensue.
- If significant neurologic compression is encountered, surgical decompression and removal of the limbus may be required to avoid late stenosis.