General
- The outcome of surgical procedures is extremely influenced by patient selection.
Principles
- Identify putative epileptogenic zone
- Through concordance of various investigation
- Determine functional consequences of resection
- De-function epileptogenic zone either by removal or disconnection
Aims
- Primary outcome aims
- Seizure freedom/reduction
- Secondary outcome aims
- Neurodevelopmental gains
- Behavioural improvement
Numbers
- Epilepsy is a common condition that affects nearly 1% of the world's population.
- WHO life lost to disability epilepsy ranks 4th
- 2/3 of patients with epilepsy achieve good control of seizures using antiepileptic medications,
- 1/3 have seizures that are resistant to medications and may be considered as candidates for epilepsy surgery.
- The benefit of epilepsy surgery in treatment-resistant epilepsy has been demonstrated in numerous case series as well as by a recent randomised clinical trial which demonstrated that surgery is clearly superior to best medical therapy in patients with temporal lobe epilepsy (TLE)
Indications
- Medically refractory temporal lobe epilepsy of mesial temporal origin.
- Medically refractory: failure of at >2 trials of antiepileptic drug monotherapy and one combination therapy over 1-2 years; AND
- Evidence implicating unilateral mesial temporal structures as the epileptogenic region
- Compatible ictal semiology
- Neurological history
- Video-EEG monitoring should confirm ictal semiology and stereotyped ictal onset on scalp EEG consistent with mesial temporal origin.
- Interictal EEG may show concordant unilateral or bilateral (usually ipsilateral predominant) epileptiform discharges.
- MRI
- Abnormality in the mesial temporal structures:
- Most commonly hippocampal atrophy with or without mesial temporal signal change on T2-weighted or FLAIR sequences.
- Mesial temporal foreign tissue lesions (e.g., low grade tumor) or neurodevelopmental abnormalities may also be good candidates for this procedure.
- Do not perform surgery for epilepsy where concordance is in investigation are not met
Pathology
- Most people with TLE have seizures that originate from the mesial-basal temporal lobe structures, including the
- Hippocampus
- Amygdala
- Parahippocampal gyrus.
- Mesial temporal lobe epilepsy-symptomatic
- Hippocampal atrophy/sclerosis
- Lesional temporal lobe epilepsy - symptomatic
- Structural lesion other than hippocampal atrophy/sclerosis
- DNT
- Ganglioglioma
- Astrocytoma
- Vascular malformations
- Hippocampal, porencephalic cysts
- Arachnoid cysts
- Tuberculomas
- Encephalomalacia
- Posttraumatic
- Dual pathology
- Extrahippocampal lesion associated with hippocampal atrophy/sclerosis
- Cryptogenic
- Non-lesional temporal lobe epilepsy
- Idiopathic
- Normal MRI-scan and/or histology
- Familial temporal lobe epilepsies
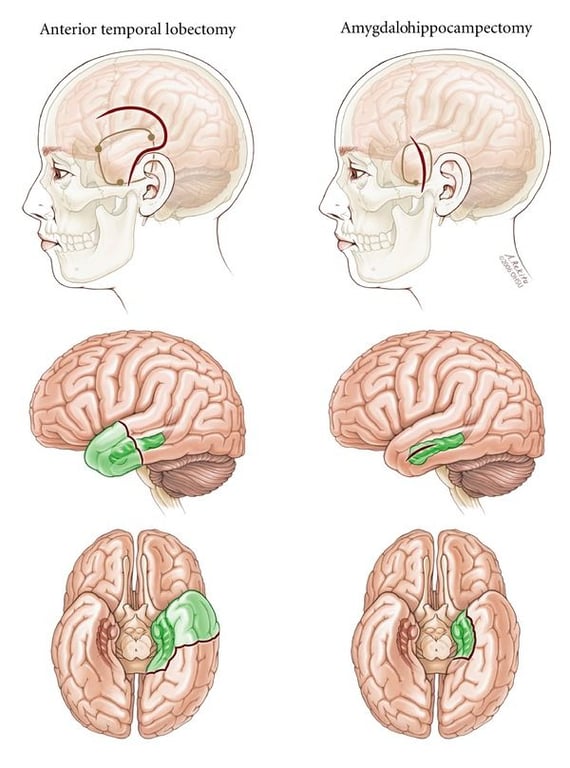
Surgical technique
- Various mesial temporal lobe approaches
Contra-indication
- Occasional patients with well-defined mesial temporal onset seizures should be excluded from consideration for SAH.
- Most patients with documented independent bitemporal onset seizures
- Those at risk for severe global memory impairment as a result of surgery.
- Patients with dominant temporal lobe foci are at greatest risk for postoperative functional decline in verbal memory, especially patients with
- High preoperative verbal memory performance,
- Normal hippocampal volume,
- Later onset of seizures in adulthood
- Patients with a similar pattern in the nondominant temporal lobe can also experience clinically important deficits, but these are usually less prominent than in dominant temporal lobe resections
- Patients with severe bilateral hippocampal atrophy who fail to demonstrate support of memory function contralateral to the proposed surgical side on intracarotid amytal procedure (Wada test) may be at risk for disabling global memory impairment,
- This is rare
- Idiopathic (primary) generalized epilepsies,
- Extratemporal focal epilepsy,
- Temporal neocortical foci or temporal lobe epilepsy not clearly localized to mesial temporal structures
- Patients with exclusively psychogenic nonepileptic seizures (PNES) are not candidates;
- Those with concurrent PNES and mTLE must be assessed very carefully, but the presence of PNES should not exclude patients a priori
Outcomes
Seizure outcome
According to aetiology
Comparing general resections
Comparing surgery vs conservative
ㅤ | Medical | Surgical |
Chance of seizure control | <5% | 70% |
Risk | - Morbidity from seizures - Psychosocial handicap - 1/100 annual mortality | - 1/100 long-lasting impairment hemiparesis, aphasia - 1/20 quadrantanopia prevents driving |
Eriksson 2023
- 859 (402 females) underwent surgical resection or disconnection at a median age of 8.5 years (IQR=4.6-13.4).
- Excluding palliative procedures, 67% of patients were seizure-free and 15% were on no antiseizure medication at one-year follow-up
Wiebe 2001:
- RCT: Surgery vs conservative
- Inclusion
- Patient >16 yrs old
- Had seizures with strong temporal-lobe semiology for > 1year.
- Seizures had to have occurred monthly, on average, during the preceding year, despite the use of two or more anticonvulsant drugs, one of which was
- Phenytoin
- Carbamazepine
- Valproic acid
- Excluded
- Tumour
- Progressive central nervous system disorders
- Active psychosis
- Pseudoseizures
- A full-scale IQ lower than 70
- Previous surgery for epilepsy,
- Focal extratemporal spikes or slowing on scalp-recorded EEG, or evidence on MRI of extratemporal lesions capable of producing the patient's seizures or of bilateral and equally severe epileptogenic lesions in the temporal lobe
- Patient who under went surgery had better seizure control
- Engel 1B for 58% of Surgery and 8% in medical group
- Surgery patient had better QOL
- P=0.003 for the trend for months 3 through 12).
- Surgery patient had similar employment and schooling (An expected transient decrease at three months is seen in the surgical group.
- More patients in the surgical group were employed or attending school at one year, but the difference was not significant (P=0.11).
Tisi 2011
- Studies involve
- 615 adults
- 497 anterior temporal resections
- 40 temporal lesionectomies
- 40 extratemporal lesionectomies
- 20 extratemporal resections
- 11 hemispherectomies
- 7 palliative procedures
- Follow-up for a median of 8 years (range 1–19)
- Findings
- 52% remained seizure free (apart from simple partial seizures [SPS]) at 5 years after surgery
- 47% remained seizure free at 10 years after surgery
- 28% seizure-free individuals had discontinued drugs at latest follow-up
Englot et al., 2012
- 80% of patients with temporal low grade tumours and epilepsy will become seizure- free following gross total tumour resections
Comparing ATL VS SAH
General
- There is little evidence to suggest that different approaches to SAH result in different seizure-free outcomes.
- There are some small reports suggesting that seizure-free outcomes following SAH are less robust in children compared with adults.
Arruda et al:
- ATL VS SAH
- N=74
- Not randomized;
- Different neurosurgeons preferred each procedure and selection of patients did not appear to be biased by clinical features.
- Both groups had equivalent seizure-free rates, and they concluded that the choice of procedure did not determine outcome;
- Seizure freedom was better predicted by
- Preoperative imaging findings and
- Underlying pathology.
Clusmann et al.
- ATL vs SAH
- N=321
- Seizure outcome
- Mainly correlated with
- Diagnosis and
- And reaffirmed the strong correlation of MRI findings and underlying pathology with outcome
- Clinical factors
- Rather than resection type
Paglioli et al
- ATL vs SAH
- N=161
- Mean follow up of 5.8 years
- No significant group differences in outcome
- Fewer patients undergoing SAH were left with isolated auras.
Mackenzie et al
- Was the exception: this study showed poorer outcomes following SAH
- However there was selection bias.
- Patients with concordant findings on noninvasive evaluations underwent ATL, while SAH was performed only in a subset of more complex cases that underwent intracranial monitoring and that were more likely to have normal MRI findings.
Abosch et al
- Reported factors that might be predictive of failure to control seizures with SAH
- Many of the signs predictive of higher risk of surgical failure following SAH are not unique to this procedure and also predict lower success rates following ATL.
- Bitemporal EEG findings
- Normal hippocampal volumes
- Use of intracranial monitoring
- In fact, those who underwent a second resection to extend the initial selective procedure largely continued to fare poorly.
Neuropsychological outcome
- Although accumulated evidence reviewed above suggests a potential cognitive benefit of the more selective procedure (SAH), it also provides ample evidence that the more selective approach does not obviate the need for careful preoperative cognitive assessment, particularly with respect to risk of verbal memory worsening following dominant temporal lobe SAH.
- The risk to verbal memory
- Depends largely on the functional adequacy of the resected tissue,
- Cognitive reserve (perhaps related in part to age and duration of epilepsy),
- Success in obtaining seizure freedom
- A lot of ATL vs SAH studies have the following issue
- Non-contemporary cohorts
- Risk of selection bias
- Nonuniform choice of cognitive assessments.
- Eg
- Some studies focused on measures specifically targeted at anticipated deficits (e.g., verbal memory tests)
- Others used extensive batteries of tests that run the risk of type I error
- While others used general measures that may be insensitive to changes caused by surgery (e.g., IQ scores).
- It is important to keep in mind that an absence of demonstrated superior cognitive outcomes with the more selective procedure does not mean that it does not produce cognitive sparing;
- An alternative explanation is that the cognitive tests may be too insensitive to detect differences.
- Recent work has identified some previously unrecognised language areas in anterior temporal neocortex that could be at risk with a standard ATL procedure, though the extent of functional sparing following SAH has been debated
- Gleissner
- Underwent SAH
- Reported
- First 3-month (N=140)
- Nearly half of the left SAH patients showed substantial loss of verbal memory
- Functional declines were less common with right-sided operations.
- 1-year findings (N= 115)
- No substantial recovery of verbal memory from the earlier time point.
- Preoperative performance was the primary predictor of postoperative performance at 1 year.
- Paglioli et al (N=161 patients) (nonrandomized, noncontemporaneous)
- ATL vs SAH
- Patients who underwent either procedure were at risk of verbal memory decline if surgery was carried out in the dominant temporal lobe;
- However, a greater proportion of left SAH patients had improved verbal memory after surgery compared with the left ATL procedure
- Clusmann
- Reported better outcome following SAH for attention, verbal memory, and a composite of total neuropsychological performance
- Tanriverdi
- SAH (n = 133) vs ATL (n = 123)
- Although both surgeries are effective, they both have the potential to cause cognitive deficits
- Lutz et al. (N = 140) randomized prospective trial of transsylvian versus transcortical SAH in a uniform population of patients with presumed mesial temporal sclerosis.
- Few differences were found in the proportions of patients in each group with neuropsychological improvement or worsening on postoperative neuropsychological tests, and left-sided surgeries resulted in worsening of verbal memory regardless of approach.
- The exception was word fluency, which improved in the transcortical but not transsylvian group.
Complications
- Gooneratne 2017
- Method
- 911 procedures: no perioperative deaths
- Persistent neurological deficit:
- Expected
- Quadrantonopia 9.4%
- Unexpected
- Quadrantonopia 0.7%
- Hemianopia 0.2%
- Hemi/monoparesis 1%
- Dysphasia 1%
- Surgical complications
- Infection 2.6%
- Hematoma 0.3%
- CSF leak 1.2%
- Visual field deficits
- Seen following ATL can also be seen with SAH, depending on the surgical approach, though they may be less severe following the more selective procedure
- Variable contralateral homonymous superior quadrant visual field defect from injury to Meyer's loop (usually asymptomatic)
- Language deficits
- Particularly dysnomia, occur less frequently
- Hemiparesis
- Uncommon (< 2%)
- Because the surgery is performed at a distance from the motor fibers of the corticospinal tract
- Other neurological problems that can occur include diplopia caused by extraocular nerve deficits and facial paresis
- Haemorrhage
- Infarction (commonly of deep penetrating vessels leading to lacunar stroke)
- Infection
- Incomplete resection
- Memory impairment
- Mood changes
Paediatric
- Options
- Cortical resection of seizure focus
- With rare exceptions, the only chance for complete seizure control is with cortical resection.
- Factors that increase chance of seizure free
- Location of seizure focus (Temporal > extra-temporal)
- For extratemporal lobe or multiple lobe resections, most series report a 50-60% good or excellent outcome at 1-2 years.
- Unlike in adults, extratemporal lobe seizure foci are more common than temporal lobe foci in children (although children with isolated temporal lobe seizure foci can expect the same excellent outcomes as adults, and better than with other causes).
- Dual pathology (i.e. a primarily extratemporal focus and secondary temporal lobe involvement) is not uncommon in children but extratemporal foci are often difficult to identify or localize.
- For example, parietal foci are notorious for being clinically silent until the seizures spread or propagate to the frontal or temporal lobes and then present as a falsely localizing semiology.
- Children are also more prone to having multiple or multilobar seizure foci. Also, due to the limitations of surface EEG probes some children with MRI lesions causing focal seizure onset are initially thought to have nonsurgical generalized epilepsy.
- Presurgical duration of seizures (shorter the better)
- A well-defined lesion (vs No lesion)
- A tumour or vascular malformation
- Palliative surgery
- For children who are not reasonable candidates for resection of the seizure focus, palliative procedures offer significant potential to improve their quality of life.
- Reducing the seizure burden by making the seizures less debilitating in some facet greatly improves their quality of life.
- Benefits of early surgery
- Offers effective treatment for children with intractable epilepsy
- Shorter the duration of uncontrolled seizures the better the outcome from surgery.
- Minimizes the disruption of a child’s cognitive and social development compared to peers,
- Decreasing the medical and traumatic risks of persistent seizures.
- SUDEP