Source:
Definition
- Radiculopathy is a neurological state in which conduction is limited or blocked along a spinal nerve or its roots
- it is differentiated from radicular pain, although they commonly occur together.
- Radicular pain is usually caused by compression of the nerve root due to cervical disc herniation or degenerative spondylotic changes, but radicular symptoms can also occur without evident compression (for example, due to inflammation of the nerve).
- Cervical radiculopathy
- pain and weakness and/or numbness in one or both of the upper extremities which corresponds to the dermatome of the involved cervical nerve root.
Aetiology
- Degenerative changes
- cervical disc herniation
- spondylosis.
Numbers
- Peak incidence:
- Aged 50 to 54 years
- Annual incidence in:
- Men is 107 per 100,000.
- Women is 64 per 100,000.
Natural Hx
- Around 88 % improve within 4 weeks with non-operative management.
Classification (Park’s method)
- T2 reconstructed oblique sagittal magnetic resonance images and schematic drawing of cervical foraminal stenosis grades 0 (AB), 1 (CD), 2 (EF) and 3 (GH).
- Grade 0 = no stenosis
- Grade 1 = mild stenosis with perineural fat obliteration < 50% of nerve root circumference
- Grade 2 = moderate stenosis with perineural fat obliteration > 50% of nerve root circumference
- Grade 3 = severe stenosis collapsed nerve root and morphological changes of the nerve root.
- CFS grade and total count were correlated with neck and arm VAS.
- Arm pain occurred more frequently on the side with more grade 2 and 3 CFS.
Clinical features
- Symptoms
- Can appear gradually or abrupt
- Pain in the neck, shoulder and/or arm that approximates to that of a dermatome.
- It is usually unilateral, but may be bilateral.
- Can be severe enough to wake the person at night.
- Sensory symptoms
- such as absent or altered sensation (for example, shooting pains, numbness, and hyperaesthesia).
- Sensory symptoms are more common than motor symptoms.
- Motor symptoms
- Muscle weakness.
- The most common nerve root affected is C7, followed by C6
- Note
- Retro-orbital and temporal pain suggest referral from the upper cervical levels (C1 to C3) and can mimic giant cell arteritis
- Signs
- Postural asymmetry
- the head may be held to one side or flexed, as this decompresses the nerve root.
- If the asymmetry is long-standing, muscle wasting may be present.
- Restricted Neck movements
- Sharp pain may radiate into the arms (especially on extension or on bending or turning to the affected side).
- Dural irritation — assess with the Spurling test.
- Neurological deficit
- Paraesthesia
- Dermatomal sensory or motor deficit,
- Diminished tendon reflexes at the appropriate level.
- Nerve root symptoms should normally arise from a single nerve root — involvement of more than one nerve root suggests a more widespread neurological disorder.
- Atypical signs of cervical radiculopathy include:
- deltoid weakness,
- scapular winging,
- weakness of the intrinsic muscles of the hand,
- chest or deep breast pain,
- headaches.
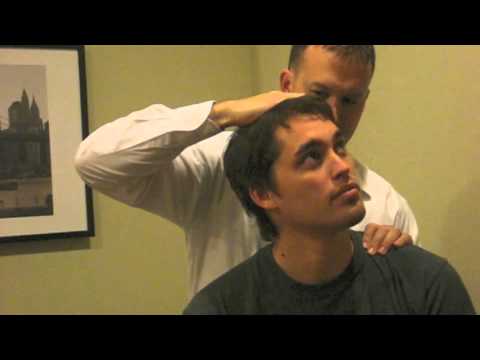
- Spurling test A and B
PURPOSE | Results of this pain provocation test are considered positive for cervical nerve root irritation if the patient reports reproduction or intensification of peripheral symptoms with application of the test manoeuvre. |
PATIENT POSITION | The patient is seated in a straight-backed chair. Having the patient face a mirror is also helpful to monitor pain facial expressions during the test. |
THERAPIST POSITION | The therapist stands behind the patient. |
PROCEDURE | Spurling test A: lateral flexion of head toward the symptomatic side and applies compressive overpressure (approximately 7 kg) to the patient’s head in the direction of the side bending to perform |
Spurling test B: combines cervical extension and rotation with ipsilateral lateral flexion. Application of overpressure for Spurling test B is the same as in Spurling test A. | |
NOTES | If the patient reports neck or arm symptom reproduction related to the condition at any point during performance of the test, results are considered positive and no further application of force is needed. Wainner et al.74 reported kappa of 0.60 (0.32, 0.87) for Spurling test A and kappa of 0.62 (0.25, 0.99) for Spurling test B. |
Spurling test B was used on 255 patients who were referred for electrodiagnosis of the upper extremity nerve disorders.105 Test results were scored positive if symptoms were reported beyond the elbow, and results were correlated with the results of the electrodiagnostic tests. The Spurling test had a sensitivity of 30% and a specificity of 93%, which means that it is not a very useful screening tool but that it is clinically useful to help confirm cervical radiculopathy.105 | |
Spurling test A is one of the four findings for the CPR for cervical radiculopathy. |

- Arm squeeze test
- This is a new clinical test that may be useful to distinguish between Cervical radiculopathy from other shoulders related pathology
- Technique
- The examiner stands behind the patient
- Squeezes the middle third of the patient's upper arm with the thumb (examiner) on the patient's triceps while the rest of the fingers is on the patient's biceps
- With a moderate compression (5.9 to 8.1kg)
- The test is positive if the patient reports 3 or higher on VAS with pressure on the middle third of the upper arm compared with the acromioclavicular joint and subacromial area
- Theory: if nerve root is irritated the distal nerves will be more sensitive to pressure on squeezing
- Arm Squeeze Test | Cervical Nerve Root Compression
- Axial traction
- Technique
- Patient lies supine and the neck is comfortably positioned. Examiner securely grasps the patient's either by placing each hand around the patient’s mastoid processes, while standing at their head, or place one hand on their forehead and the other on the occiput. Slightly flex the patient’s neck and pull the head towards your torso, applying a distraction force
- If pain is relieved as a result of the movement, then the test is positive for nerve root compression and facet joint pressure.
- Distraction Test
- Upper limb neurodynamic tests — a combination of four neurodynamic tests and an arm squeeze test can rule out cervical radiculopathy.
- Shoulder abduction test/ Bakody test
- Procedure
- subject could be sitting or lying down.
- The upper limb is actively or passively raised above the head with the palm of the hand touching the head.
- Positive sign:
- Reduction in symptoms with the painful arm placed on top of the head.
- The suggested mechanism includes reduction of pain as the traction force to the nerves and the lower brachial plexus trunks are relieved.
- With the arm hanging at the side of one's body, the mechanical traction acting on the nerve increases, thus increasing symptoms. [4][5]
- Negative sign:
- Increase in the symptoms when the patient's hand is placed on the head.
- These symptoms are probably increased due to inter-scalene muscle compression.
- Thus placing the hand could be termed positive for inter-scalene compression and negative for Bakody sign
Imaging
- Cervical X-rays and other imaging studies and investigations are not normally required to diagnose or manage cervical radiculopathy.
- MRI
- If cervical radiculopathy which has been present > 4–6 weeks or objective neurological signs
Treatment
Conservative
- Indicated
- For people who have neck pain for less than 4–6 weeks
- no objective neurological signs
- Rest, medications, and rehabilitation
- Indications
- 75% of patients with radiculopathy improve with nonoperative management
- improvement via resorption of soft discs and decreased inflammation around irritated nerve roots
- Considering a referral for physiotherapy.
- Engquist et al., 2013
- surgery with physiotherapy resulted in a more rapid improvement during the first postoperative year, with significantly greater improvement in neck pain and the patient's global assessment than physiotherapy alone, but the differences between the groups decreased after 2 years. Structured physiotherapy should be tried before surgery is chosen.
- Outcome
- >90% have improvement in their arm symptoms.
- Providing reassurance, information and advice.
- Offering oral analgesia to relieve symptoms.
- Considering offering amitriptyline, duloxetine, pregabalin or gabapentin.
- Return to play
- indicated after resolution of symptoms and repeat MRI demonstrating no cord compression
- studies have shown return to play expedited with brief course of oral methylprednisolone
- no increased risk of subsequent spinal cord injury
- Selective nerve root corticosteroid injections
- Indications
- may be considered as therapeutic or diagnostic option
- outcomes
- provides long-term relief in 40-70% of cases
- increased risk when compared to lumbar selective nerve root injections with the following rare but possible complications, including
- dural puncture
- meningitis
- epidural abscess
- nerve root injury
- Evidence
- Persson 1997 RCT n81: Surgery (ACDF) improves pain and motor/sensory symptoms in the short term (3months) but in the long term (16 months) surgery is not better than conservative (collar/physiotherapy)
Surgery
- Indication
- Radicular signs and symptoms, in one or both arms (pain, paresthesia or paresis in a specific nerve root distribution)
- For at least eight weeks and for whom conservative therapy (no physiotherapy or injections were prescribed) failed
- Severe or progressive neurological deficits
- Deltoid palsy
- Triceps palsy
- Wrist drop
- Hand intrinsic muscle weakness
- Decision tree
- Theodore 2001
- Algorithm for treatment options for patients with radiculopathy.
graph TD A[Radiculopathy] --> B{No axial pain} A[Radiculopathy] --> C{Axial pain} B --> D{Normal lordosis} B --> E{Abnormal lordosis} C --> F{1 or 2 levels} C --> G{3 levels or more} D --> H[Lateral disk herniation] D --> I[Centrolateral disk herniation] E --> J[ACDF or ACDFPa] F --> J H --> K[PCD, ACD, ACDF, or ACDFPa] I --> L[ACD, ACDF, or ACDFPa] G --> M[ACDFP]
ACD, anterior cervical discectomy; ACDF, anterior cervical discectomy with interbody fusion; ACDFP, anterior cervical discectomy with interbody fusion and an anterior plate system with screws; PCD, posterior cervical discectomy.
- Anterior cervical discectomy and fusion
- Indications
- persistent and disabling pain that has failed three months of conservative management
- progressive and significant neurologic deficits
- static neurologic deficit associated with significant radicular pain
- Outcomes
- Remains gold standard in surgical treatment of cervical radiculopathy
- Very high success rate with single level disease
- Higher rate of pseudoarthrosis with multilevel procedures
- 20% for single level ACDF vs >50% for multilevel ACDF
- Pseudoarthrosis rate does not appear to correlate with clinical outcomes
- Anterior cervical foraminotomy
- Indications
- isolated unilateral nerve root compression
- high risk patients for pseudoarthrosis
- smokers
- Diabetics
- Techniques (jho procedure)
- Done under microscope or endoscope
- compressive pathology is directly removed via an anterior approach while the remaining disc and functioning motion unit is preserved without the use of implants or bone fusion.
- Removing the uncovertebral juncture (the most lateral part of the intervertebral disc) to access the compressive pathology.
- Soft disc and/or bone spurs that compose the compressive pathology are excised
- Pros
- avoids fusing the involved level
- Cons
- potential risk of sympathetic chain and vertebral artery injury
- outcomes
- limited studies
- not widely accepted
- 98% excellent outcomes reported in literature
- Posterior foraminotomy
- Avoid resecting over 50% of the facet otherwise this could lead to instability.
- Indications
- Foraminal soft disc herniation causing single level radiculopathy ideal
- May be used in osteophytic foraminal narrowing
- Failed nonoperative treatment
- High risk patients with anterior approach
- previous anterior surgery
- abnormal anatomy
- Contraindications
- Large central disc herniation
- cervical myelopathy
- instability
- OPLL
- Do not perform bilateral foraminotomy if
- kyphotic deformity
- Outcomes
- >91% success rate
- reduces the risk of iatrogenic injury with anterior approaches
- low complication rate
- ~3%
- no difference in outcomes compared to ACDF
- faster return to work and lower treatment cost than ACDF
- Evidence
- Post foraminotomy (PCF) vs ACDF
- Zou 2022 meta-analysis
- Minimal invasive PCF is cheaper and has shorter postoperative hospitalization time compared to ACDF
- Operation time, complication/reoperation rate, and VAS-arm, VAS-neck, and NDI scores were comparable between the two cohorts.
- FACET trial 2023 RCT N265
- PCF is not inferior to ACDF in terms of arm pain outcomes
- Cervical disc arthroplasty
- indications (controversial)
- single level disease with minimal arthrosis of the facets
- outcomes
- Goedmakers 2023 (NECK trial)
- ACDFusion vs ACDArthoplasty:
- 5 yrs after surgery:
- Similar clinical results
- ACDA does not have less reoperations at adjacent level
- Do not perform ACDiscectomy only (no implants)
- Worse clinical outcome and pain
- Hypothesis: caused by delayed fusion
- Emphasis on need for focus on timely fusion in future research
- NORCAT (Norwegian Cervical Arthroplasty Trial)
- 2-year clinical outcome
- clinical C6 or C7 radiculopathy with corresponding radiological findings,
- Single-level cervical arthroplasty VS cage fusion
- single-blinded, randomized, controlled multicenter study
- N136
- No observed significant between-group
- Self-rated Neck Disability Index
- Pain and quality of life questionnaires
- Short Form-36
- EuroQol-5Dimension-3 Level
- Effect on adjacent level disease remains unclear
- some studies show 3% per year for all approaches
- systematic reviews have demonstrated no difference in ASD rate between CDA and ACDF
- Lower reoperation rates seen with CDA
- Lower neck pain intensity and frequency with CDA
- High incidence of heterotopic bone formation
- 60% of cases
- No effect on motion profile