Definition
- The migration of fibrocartilaginous nucleus pulposus material through the nearby vasculature to embolize into one of the spinal cord vessels
Numbers
- female predominance (63.5% female vs 36.5% male)
- Age
- Range 14-78 years
- Average 41years
- Half of the patients were under 40 years of age
Clinical presentation
- Like any spinal cord infarction
- onset of dull transient neck or back pain followed by or accompanying a syndrome of myelopathy.
- Has a sensory level
- A pathognomonic clinical finding for anterior spinal artery infarction is the sparing of proprioception and vibratory sensation below the sensory level.
- bladder and/or bowel dysfunction
- Paraplegia or Quadriplegia
- Possible respiratory compromise for higher than C5 cervical cord disease.
- Temporal
- Infarction versus Inflammatory
- Infarction has rapid course of symptoms to nadir, typically over hours.
- A characteristic clinical symptom that may point to FCE as a cause for this spinal cord infarction is a temporal correlation with a minor or even unnoticed incident that triggers the increased intra-disc or intra-vertebral body pressure as described above in the “Mechanisms” section.
- In our review of tissue diagnosed FCE
- 61% of the cases presented following such an event.
- The duration between this trigger event and the onset of symptoms varied from minutes to days, but averaged at 2.4 days.
- The weakness was asymmetric in 15% of the cases.
- There was associated neck or back pain in 76%.
- Nearly 40% of deaths were due to preventable respiratory complications ( pulmonary embolism 20%, pneumonia 17%, aspiration 2%).
Localization
- Spine (most commo)
- Lung
- Brain
- Vertebrae and ribs
Clinical anatomy
- Disc
- In adults
- Largest avascular structure in the body
- It has also been postulated that remnants of vascular channels can persist in the inter-vertebral disc beyond the second decade of life.
- Normally
- Neo-vascularization reappears in the normal adult inter-vertebral disc at the circumferential edges at around 50 years of age.
- Degenerative disc disease
- Neo-revascularization
- occur earlier than 50
- is more pronounced
- In neonates
- highly vascular structure with large thin walled blood channels running mainly in the cartilage end plate
- Vascular tissue
- quickly starts to regress after 2 months old
- By age 11–16 years will have completely disappeared
- Can indeed be the source of embolic material as evidenced by histopath
- Annulus fibrosus
- Outer
- Mesodermally
- Nucleus pulposus
- Endodermally
- Vertebral body and the spinal cord
- have a fixed blood supply throughout life.
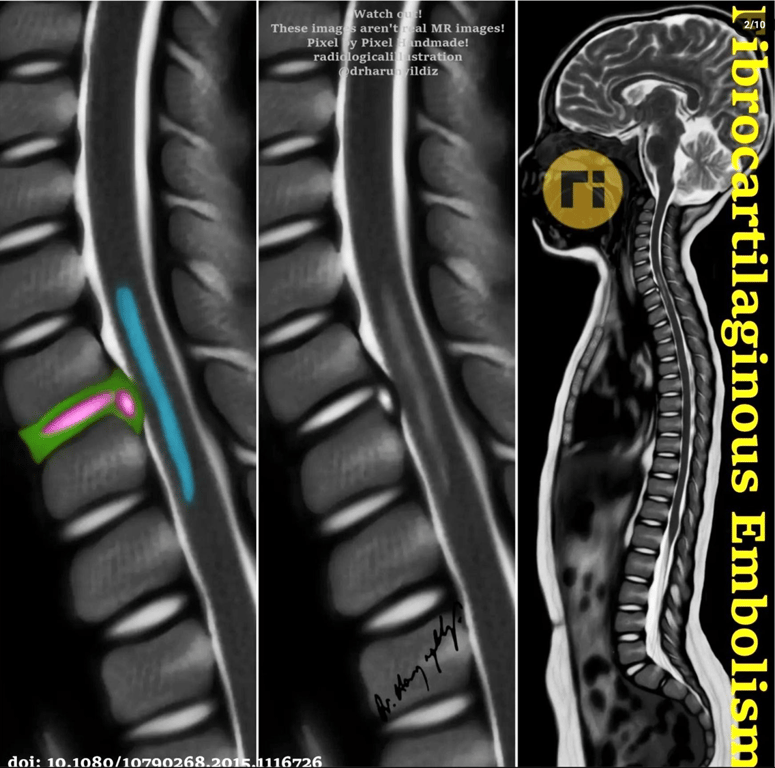
- Spinal cord
- from medulla to conus has
- One anterior longitudinal spinal arteries
- Two posterior longitudinal spinal arteries
- Radicular arteries (Ka) supply both the spinal cord and then vertebral body
- Schmorl’s nodes
- Focal masses of fibrocartilage found within the bone of vertebrae
- lie in close proximity to the vascular supply of the vertebral body.
- Common
- present in 38% to 79% of the adult population
- Developed due to herniation of nucleus pulposus material into the body of the adjacent vertebra as a consequence of degenerative disc changes
Mechanisms
- The fibrocartilaginous disc material gains vascular access via any of three pathways:
- Revascularization of the inter-vertebral disc
- by
- Normal aging
- Degenerative disc disease especially herniation;
- Initial trigger for break off of fibro-cartilaginous nucleus pulposus material is increased intra-disc or intra-vertebral body pressure by axial loading forces applied to the spine
- Such as
- Heavy lifting
- Straining
- Falls or minor traumatic events to the neck and back.
- Formation of Schmorl’s nodes
- Persistence of inter-vertebral disc vasculature into adulthood.
- Once in the vasculature, the fibrocartilaginous embolus can enter the spinal cord via either an
- Arterial route
- The fibrocartilaginous material travels retrograde through the arterial system supplying the spinal column, to reach the radicular artery which carries it into the spinal cord arterial system in a normal anterograde fashion
- Venous route
- The fibrocartilaginous material gain access to the venous system of the spinal column and travel initially in a normal anterograde fashion where they would enter the caval system, but then travel retrograde to the venous plexus of Batson and the parenchyma of the spinal cord.
- Retrograde flow in the venous route is postulated to be aided by concomitant increases in the intra-thoracic or intra-abdominal pressure as may occur with lifting, straining, coughing or valsava
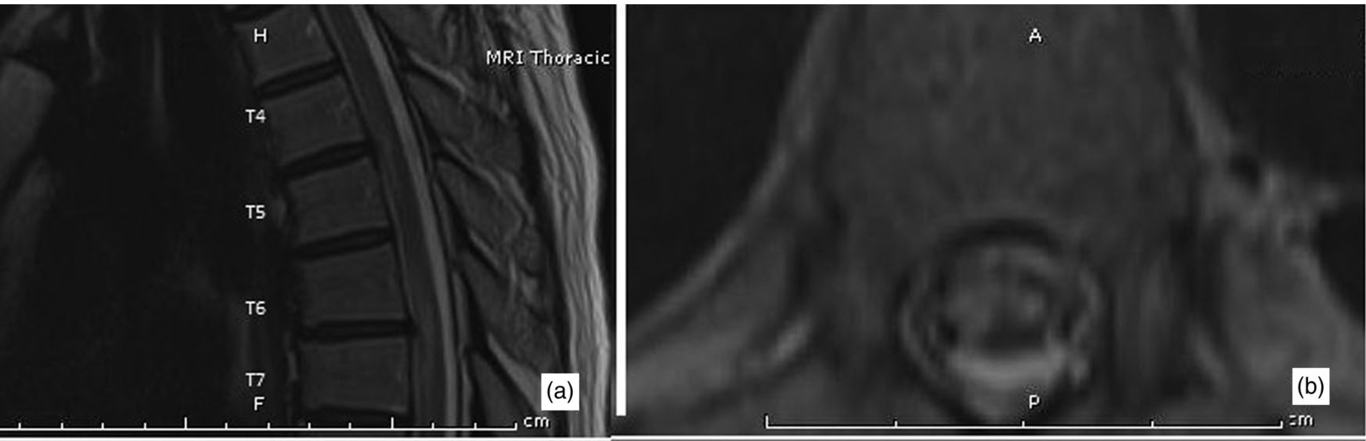
Imaging