General
- A slow growing, benign tumor
- AKA: neuroepithelial cysts
- LP is CI due to herniation risk
Numbers
- 2% of gliomas
- 0.5–1% of all intracranial tumors
- Age of diagnosis: 20–50 yrs
Localisation
- Most commonly found in the third ventricle in the region of the foramina of Monro, but may be seen elsewhere, e.g. in septum pellucidum
- Most common 3rd ventricular tumour
Pathogenesis
- Origin unknown
- Few theories but the paraphysis is the most supported
- Paraphysis: evagination in roof of third ventricle, rudimentary in humans
- Derive from abnormal folding of the primitive neuro-epithelium which in this area separates the telencephalon from the diencephalon.
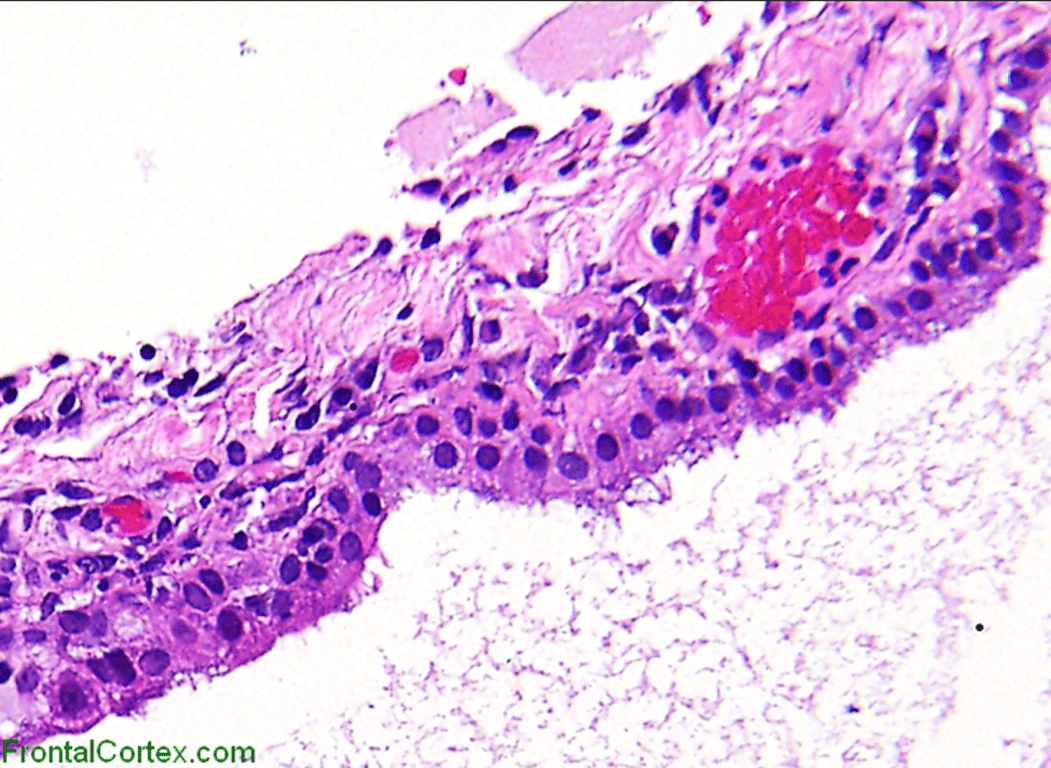
Histopathology
Macroscopic
- Unilocular round structure filled with viscous material.
Microscopically
- Unicellular cell wall
- Composed of columnar epithelium, which may or may not be ciliated.
- The epithelial cyst wall stains positive for keratin and epithelial membrane antigen (EMA).
- Cyst contents:
- Void of living cells and composed of desquamated ghost cells and filamentous material.
- Gel density material which contains mucin, cholesterol, and hyaloid substances.
- The mucin stains are positive for periodic acid-Schiff (PAS).
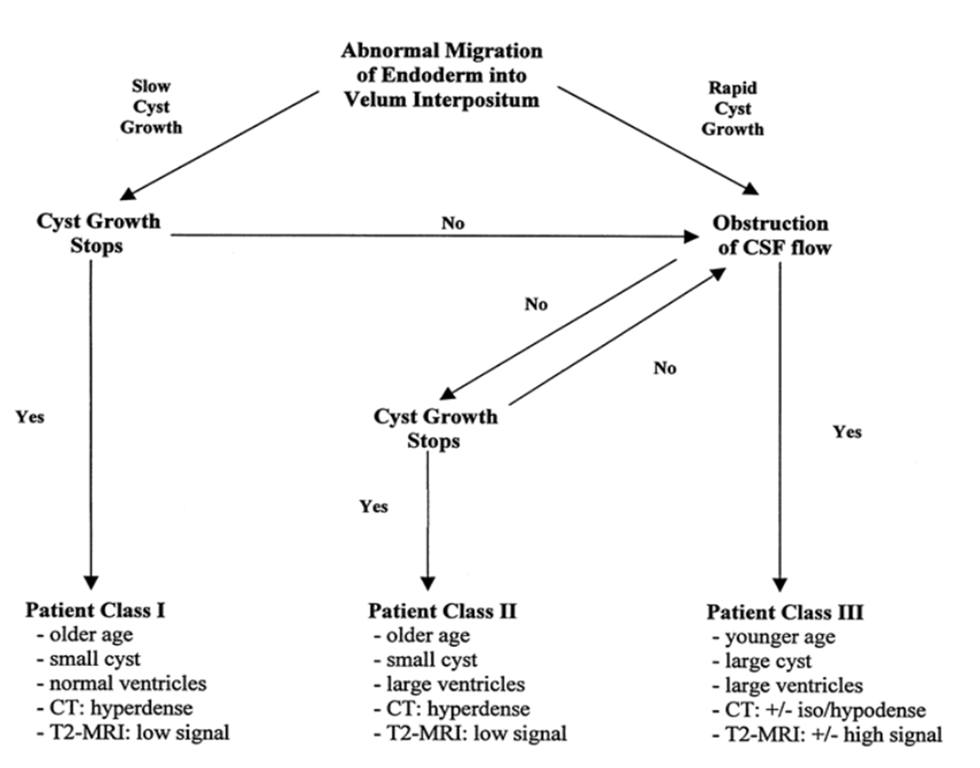
Natural history
Pollock
- 58 patients of asymptomatic patients (ave age 57: older than most patients normal mean is 47 yrs)
- Class 1 (12% have cyst related symptoms)
- Class 2 (50% have cyst related symptoms)
- Hardest to manage
- As old and also have large ventricles
- Pollock feels
- Patients with colloid cysts and enlarged ventricles can be conservatively managed if the imaging features of the cyst suggest that it has stopped growing
- Class 3 (85% have cyst related symptoms)
- Most colloid cysts stop enlarging as the patient ages
Year post incidental finding | Incidence of symptomatic worsening |
2 | 0% |
5 | 0% |
10 | 8% |
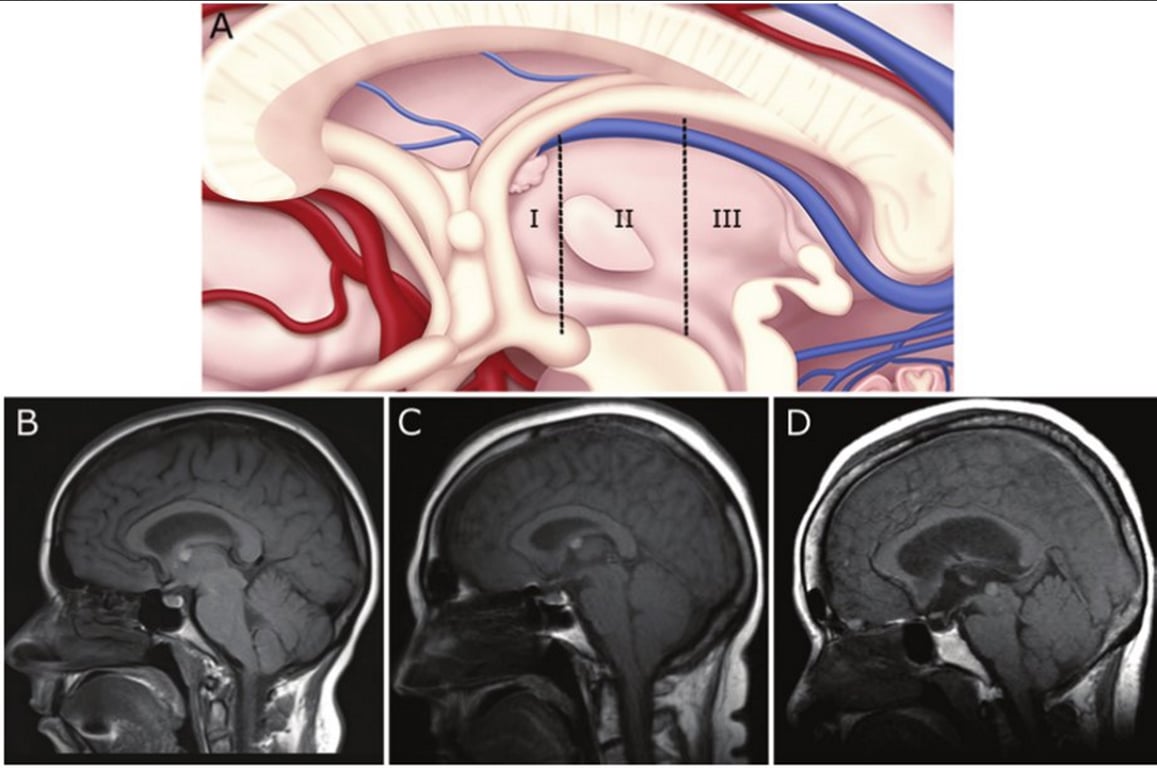
Colloid cyst risk score-Beaumont et al 2016
- Risk zones: measured on T1 are zone 1 and 3 only
- Zone I, from the lamina terminalis to a vertical line drawn from the mammillary body and tangential to the massa intermedia
- Zone II, from the posterior boundary of Zone I to the rostral apex of the midbrain tegmentum at the inlet of the cerebral aqueduct
- Zone III, from the posterior boundary of Zone II to the posterior limit of the third ventricle
- Beaumont talks about 3.1 percent mortality if you have symptomatic colloid cyst.
Criterion | Points |
Age <65 years | |
Yes | 1 |
No | 0 |
Headache | |
Yes | 1 |
No | 0 |
Axial diameter ≥7 mm | |
Yes | 1 |
No | 0 |
FLAIR hyperintensity | |
Yes | 1 |
No | 0 |
Risk zone | |
Yes | 1 |
No | 0 |
Patient stratification on Colloid cyst risk score:
CCRS | Symptomatic No. (%) | Hydrocephalus No. (%) |
0 | 0 | 0 |
1 | 0 | 0 |
2 | 1 (6) | 0 |
3 | 4 (22) | 0 |
4 | 10 (67) | 3 (20) |
5 | 24 (96) | 15 (60) |
Clinical features
- Intermittent acute intracranial hypertension
- Due to movement of the cyst on its pedicle → episodic obstruction of the foramina of Monro
- Not due to chronic hydrocephalus
- Most cysts < 1cm diameter do not produce hydrocephalus and are asymptomatic
Symptom | % | Sign | % |
Headache | 68 | Papilledema | 47 |
Gait disturbance | 47 | gait disturbance | 32 |
Reduced GCS | 37 | normal exam | 26 |
Vomiting (± nausea) | 37 | hyperreflexia | 24 |
Blurred vision | 24 | Babinski reflex | 21 |
Incontinence | 13 | incoordination | 13 |
Dizziness | 13 | Nystagmus | 13 |
Tinnitus | 13 | Tremor | 10 |
Seizures | 10 | hyporeflexia | 8 |
Diplopia | 10 | 6th nerve palsy | 5 |
- Sudden death
- High rare 20% → possibly overestimation in pre CT era
- Due to
- Disturbance of hypothalamic-mediated cardiovascular reflex control
- Procedure associated herniation (LP, ventriculography)
- Progressive obstruction from tumour growth → chronic hydrocephalus → brain decompensate at some point
- Haemorrharge within cyst à sudden expansion
- Traumatic detethering of the cyst à blocking aqueduct
- Ball valve effect does not cause death
- Many “asymptomatic” patients may have headaches at diagnosis.
- Careful evaluation of headache aetiology (i.e., posttraumatic, migraines, tension, etc.) should be undertaken to determine whether the headaches are due to the colloid cyst or if the cyst is asymptomatic
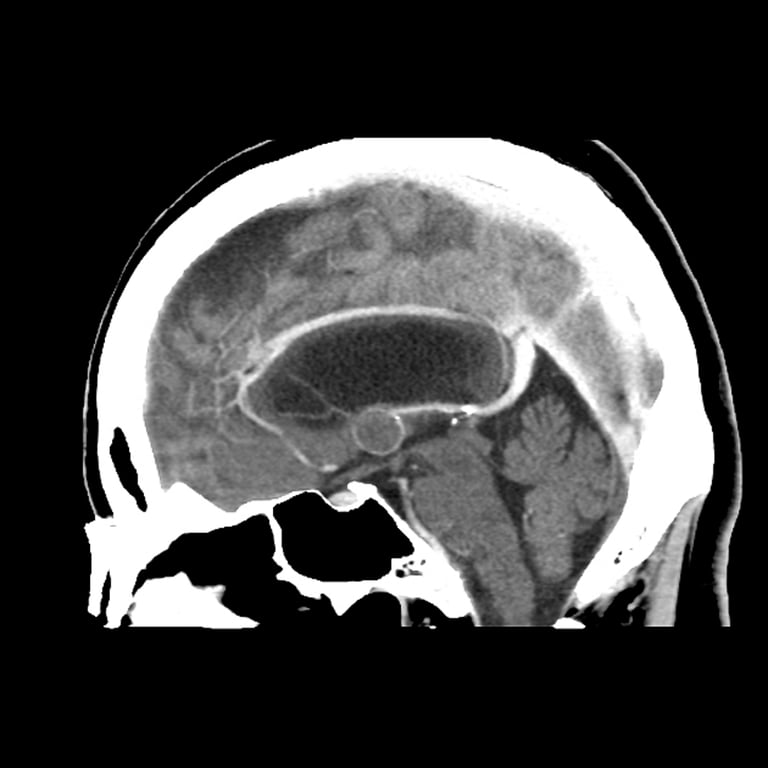
Imaging
General
- MRI > CT @ dx
- Cases where cysts are isointense on MRI and CT is superior
- CT is usually not quite as good as MRI, especially with isodense cysts.
Viscosity is correlated on CT not on MRI - Hyperdensity: high viscosity - Hypodensity: low viscosity | Fluid content is correlated on MRI T2 not on CT - Hyperintensity: high fluid levels - Hypointensity: low fluid levels |
- A rounded, sharply demarcated lesion
- At the foramen of Monro (roof of the 3rd ventricle)
- Size: 4 mm to 4 cm
- Do not
- Calcify
- Restrict diffusion
- Create brain oedema
- Enhance
CT
- Unilocular
- Hyperdense
- Isodense and hypodense cysts are uncommon
Images
CT

CT+C

MRI
- T1:
- Variable
- 50% high signal
- The rest are hypointense or isointense to adjacent brain
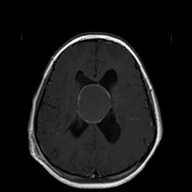
- T1 C+ (Gd):
- Only rarely demonstrates thin rim enhancement, but usually this represents an enhancement of the adjacent and stretched septal veins
- T2: variable
- Most are of low T2/T2* signal (short T2), related to thick "motor oil" consistency fluid
- Some have central low T2 and high peripheral T2 signal
- Some are homogeneously high signal
- Indicating higher water content → a propensity for continued cyst expansion → symptomatic patients
- FLAIR:
- Cysts which are of low signal on T2 will appear similar to attenuated CSF on FLAIR, and are thus difficult to appreciate
Images
T1
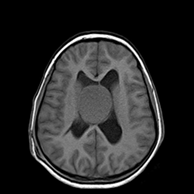
T1+C
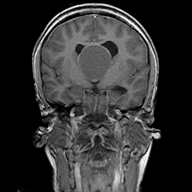

T2
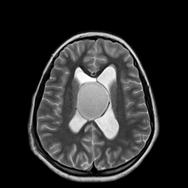
Flair
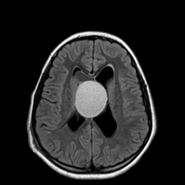
DWI

Treatment
General
- Optimum treatment is controversial
Indication
- To prevent shunt dependency → achieve patency of ventricular system
- To reduce the possibility of tumor progression
- Since the mechanism of sudden neurologic deterioration may be due to factors such as cardiovascular instability from hypothalamic compression and not due to hydrocephalus
Who to operate on
- Pollock et al: Classes of colloid cyst based on recursive partitioning analysis
- Asymptomatic patients with low T2 signal-containing cysts may reflect a group with low potential for cyst expansion and development of cyst-related symptoms (even in the presence of ventriculomegaly) → thus they may represent a population that may be safely managed in a nonoperative fashion
- Most people will operate with ventriculomegaly
Class | Age (years) | Cyst diameter | Ventricles | Symptomatic patients (% of total) | Treatment options |
I | any | ≤ 10 mm | Normal | 12% | May be monitored clinically and with serial imaging (CT or MRI) |
II | > 50 | ≤ 10 mm | Ventriculomegaly | 50% | If asymptomatic, may be monitored clinically and with serial imaging (CT or MRI) |
III | Any | > 10 mm | Normal | 85% | Surgical removal is recommended |
ㅤ | ≤ 50 | Any | Ventriculomegaly | 85% | Surgical removal is recommended |
ㅤ | > 50 | > 10 mm | Ventriculomegaly | 85% | Surgical removal is recommended |
Surgical options
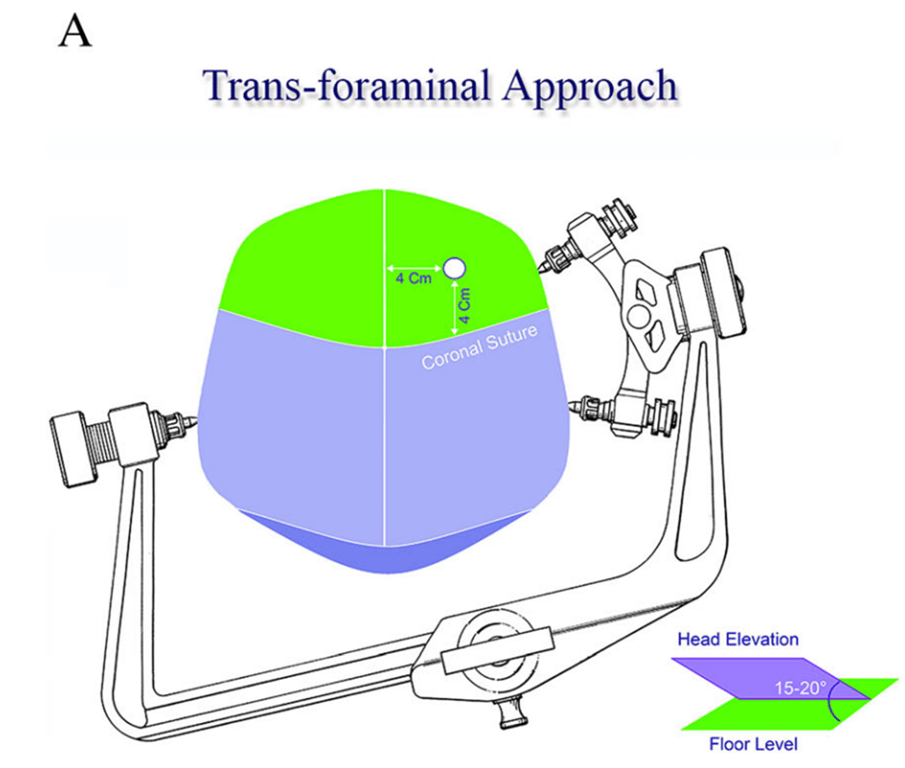
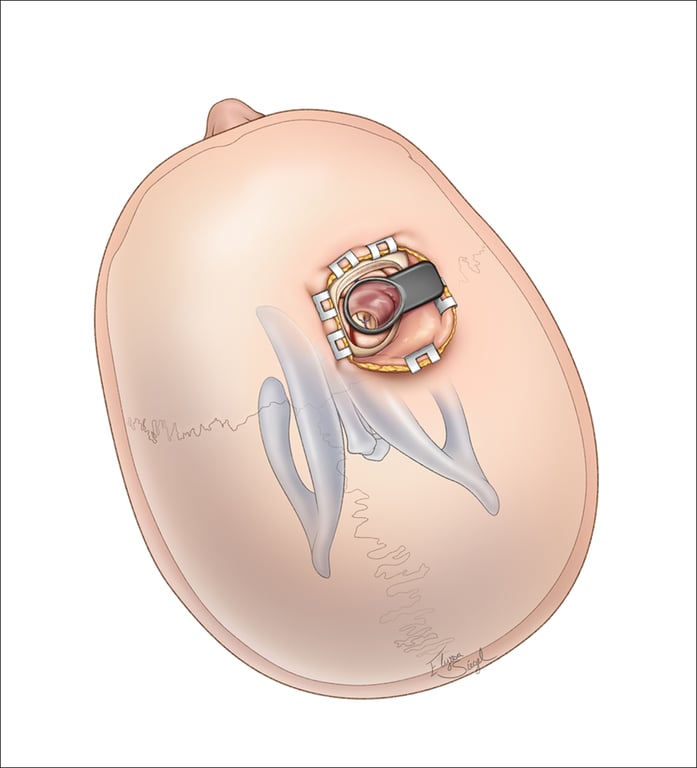
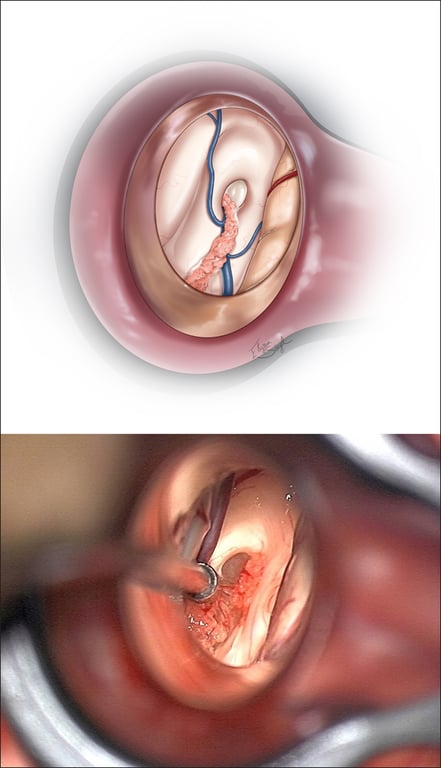
Endoscopic
Transforaminal
- Used if cyst is not occluding the foramen of munro
- Burr hole made 4 cm anterior to coronal and 4 cm lateral to midline
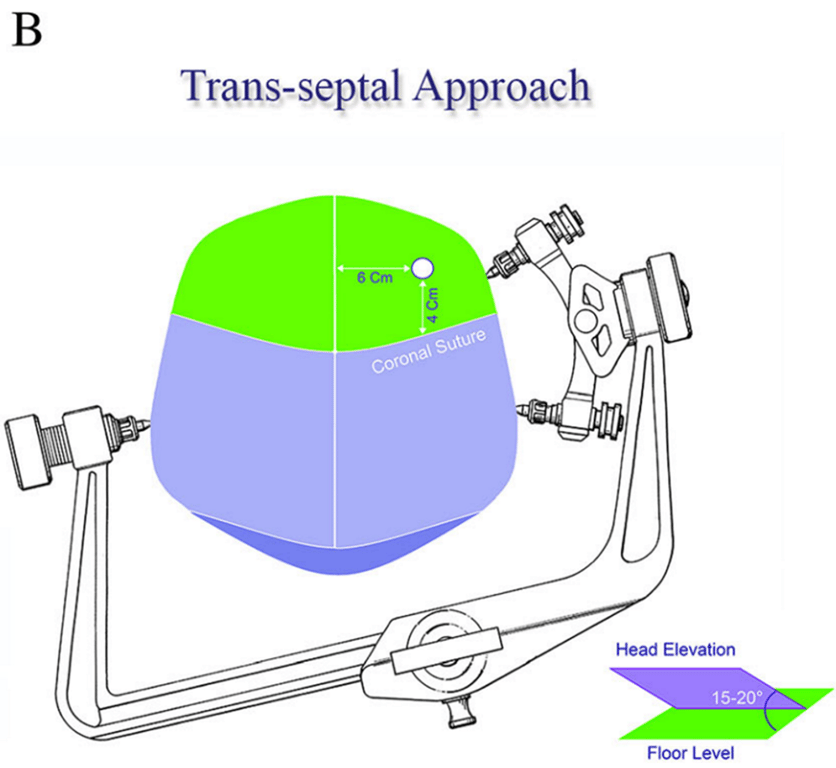
Transseptal
- Used if cyst is occluding foramen of munro
- Large cyst and grows superiorly beyond the level of the roof of the 3rd ventricle within leaflets of septum pellucidium
- Burr hole made 4 cm anterior to coronal and 6cm lateral to midline
Microscopic
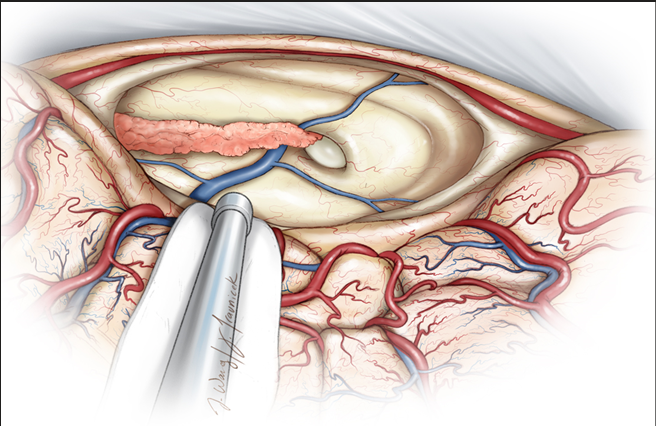
Transcallosal approaches
- Lateral position: gravity assisted retraction
- Midline horseshoe incision
- 1.5cm callosotomy
- Access to 3rd ventricle via
- Foramen of Munro
- Interfornical approach
- To inc. space for dissection
- Deflating cyst
- Fenestrate the septum pellucidum
- The capsule is primarily adherent along the choroidal fissure.
- Pros
- Not dependent on dilated ventricles.
- Cons
- Higher incidence of venous infarction or forniceal injury
Transcortical approach
- If there is ventriculomegally can be used
- Pros
- No callosotomy
- Cons
- Higher incidence of post-op seizures (≈ 5%).
- Not feasible with normal sized ventricles (e.g. in patient with VP shunt)
- Poor working angles
Stereotactic drainage
- Pro
- Useful for patients with normal ventricles from shunting
- Total or even subtotal aspiration may not require further treatment in some patients
- Cons
- Too viscous for drainage
- Tough capsule may be hard to penetrate blindly
- High recurrence rate
- Relatively high early morbidity due to
- Vascular injury
- Mechanical trauma
- Higher risk of treatment failure
- High viscosity:
- Correlates with hyperdensity on CT
- (Low viscosity correlated with hypo- or isodense CT appearance; no MRI finding correlated with viscosity)
- Deflection of the cyst from tip of aspirating needle due to small size
- Stereotactic technique:
- Insertion point of stereotactic needle is just anterior to right coronal suture
- Start with sharp-tipped 1.8mm probe, and advance to 3–5mm beyond target site (to accommodate for displacement of cyst wall)
- Use a 10ml syringe and apply 6–8ml of negative aspiration pressure
- If this does not yield any material, repeat with a 2.1mm probe
- Although complete cyst evacuation is desirable, if this cannot be accomplished an acceptable goal of aspiration is re-establishment of patency of the ventricular pathways (may be verified by injecting 1–2 cc of iohexol)
Outcome
Feature | Endoscopic | Microsurgical |
Extent of resection | 58.20% | 96.80% |
Rate of recurrence | 3.91% | 1.48% |
Reoperation rates | 3.00% | 0.38% |
Mortality (no diff) | 0.60% | 1.40% |
Shunt dependency (no diff) | 3.90% | 6.20% |
Complication | 10.50% | 16.30% |
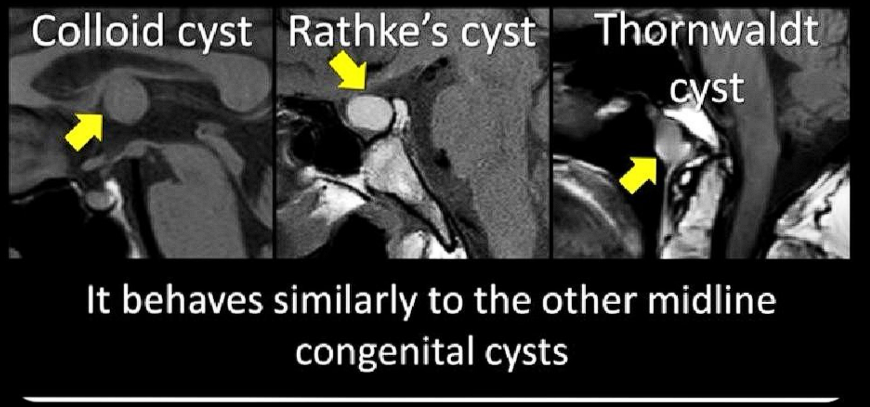
Differential diagnosis
- Masses in foramen of munro
Paediatric | Adult |
Choroid plexus papilloma | Aneurysm |
Craniopharyngioma | Colloid cyst |
Germinoma | Cysticercus cyst |
Glioma | Ependymal cyst |
Langerhans cell histiocytosis | Glioma |
Neurofibromatosis | Lymphoma |
Pilocytic astrocytoma | Meningioma |
Subependymal giant cell astrocytom | Metastasis |
ㅤ | Pituitary adenoma |
- By Lea Alhiilali