General
- Aka:
- Cholestatoma
- Pearly tumor
- Ectodermal inclusion cyst
Numbers
- 1% of intracranial tumors,
- 7% of CPA tumors.
- Peak age of occurrence: 40 years.
- No gender difference
Pathophysiology
- Epidermoid vs cholesteatoma
- Both are same but just in different places
- Both near petrous part
- Both arise from epithelium entrapped in an abnormal location
Features | Cholesteatoma | Epidermoid |
Location | Extradural (middle ear) | Intradural |
Origin
- Displaced dorsal midline ectodermal cell rests trapped during neural tube closure between gestational weeks 3–5
- Multipotential embryonic cell rests
- Epithelial cell rests carried to the Cerebral-Pontine Angle with the developing otic vesicle
- Epidermal cells displaced into CNS by
- LP or
- Repeated percutaneous cranial subdural taps
Localisation
- Intradural: 90%
- Cerebellopontine angle: 40-50%
- 3rd most common CPA mass, acoustic schwannomas>meningiomas>epidermoid cyst
- Accounts for approximately 5-10% of all tumours in this region
- Suprasellar cistern: 10-15%
- Fourth ventricle: 17%
- Middle cranial fossa
- Interhemispheric: < 5%
- Spinal (rare)
- Extradural: 10%
- Most within skull
Natural history
- Chronic
- Slow growth causing mass effect once large
- Acute
- Cyst haemorrhage and rupture causing chemical meningitis, headache, seizures, vasospasm and death
- Malignant Transformation to Squamous cell carcinoma
- Rare
- OS 9 months
- A deterioration in the absence of hydrocephalus and rapid tumour recurrence
Clinical presentation
- May present as any mass lesion in the same location
- CPA lesions can produce V, VII, or VIII neuropathies
- Recurrent rupture of cyst contents → recurrent episodes of aseptic meningitis → hydrocephalus.
- S&S of aseptic meningitis
- Symptoms include fever and meningeal irritation.
- CSF shows
- Pleocytosis
- Hypoglycorrhachia
- Elevated protein
- Negative cultures
- Cholesterol crystals may be seen: amorphous birefringent appearance.
- Mollaret’s meningitis
- A rare variant of aseptic meningitis
- Large cells in the CSF that resembling endothelial cells (which may be macrophages), which may be seen in some patients with epidermoid cysts
Imaging
General
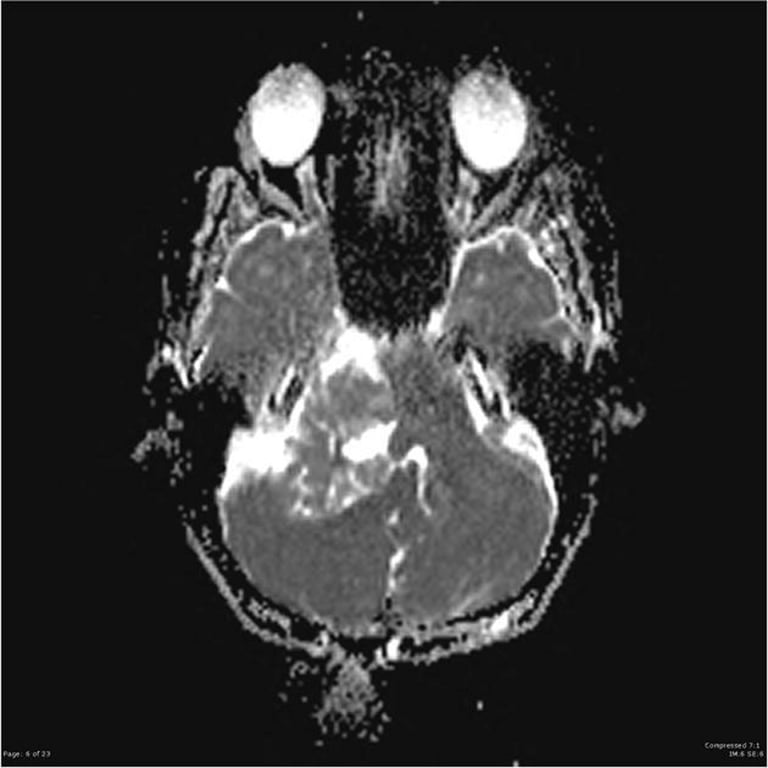
- Lobulated mass that fills and expand CSF spaces and exert a gradual mass effect
- Encase nerve and vessels
- Common feature of post fossa cyst → displacement of basilar artery away from pons
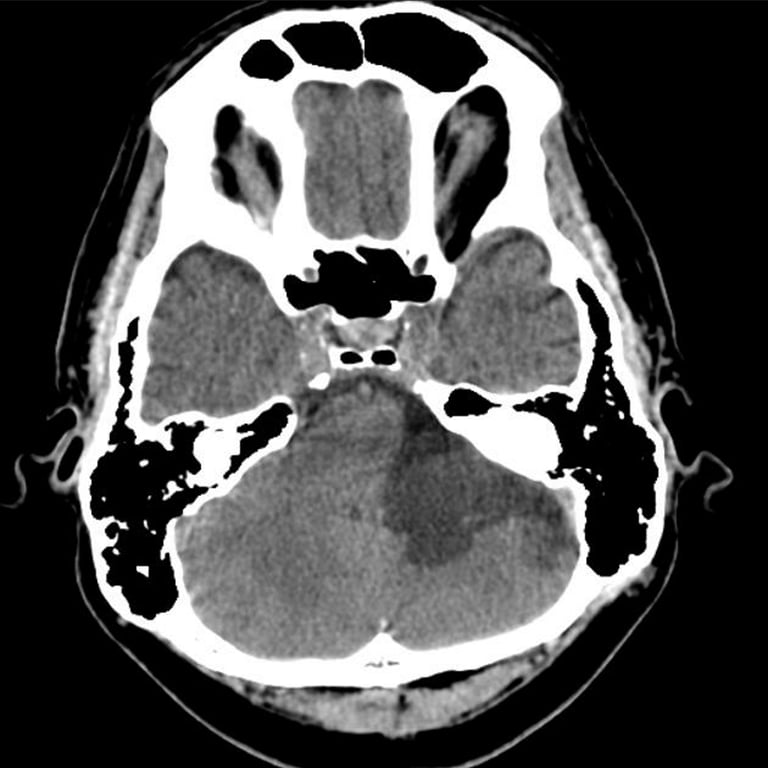
CT
- Isodense to CSF:
- Due to
- Combination of cellular debris along with a high cholesterol content lower the density of epidermoids to approximately 0 HU, and can thus be identical in density to CSF, and look the same as an arachnoid cyst.
- Calcification
- A minority of cases (10-25%)
- Rarely an epidermoid cyst may be hyperdense due to haemorrhage, saponification or high protein content ("white epidermoids"). The interhemispheric epidermoids are reported to have peripheral calcification.
- They do not enhance and only very rarely demonstrate any enhancement of the wall.
- Bone erosion in 33%
- Common location
- Uncommon locations


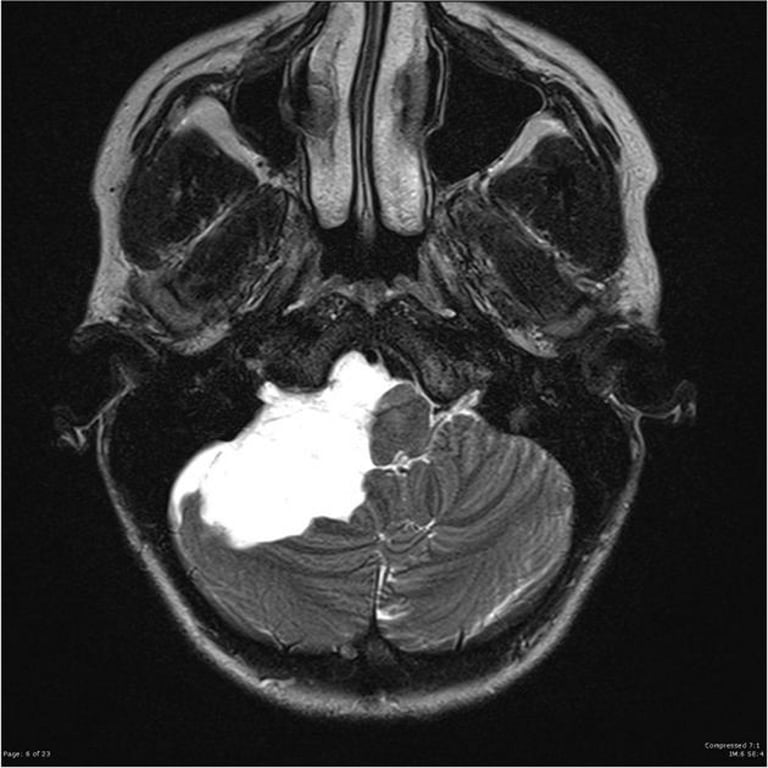
MRI
- General
- Epidermoids are often indistinguishable from arachnoid cysts or dilated CSF spaces on many MR sequences,
- Due to epidermoid cystic contents are composed of keratin, cholesterol crystals, and desquamated epithelial cells suspended in a fluid medium that closely mimics the signal characteristics of cerebrospinal fluid. This composition makes the lesion fluid-like in behavior on conventional MRI sequences, resulting in hypo-intensity on T1 and hyper-intensity on T2, similar to CSF.
- Except for DWI/ADC which helps to differentiate them.
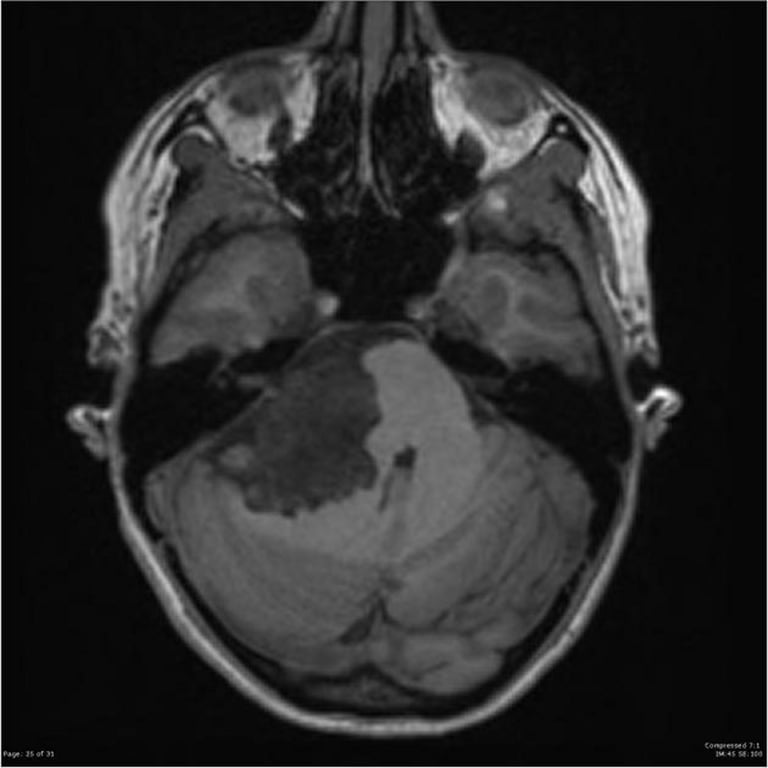
- T1
- Isointense to CSF
- Higher signal compared to CSF around the periphery of the lesion is frequently seen
- White epidermoid
- Rare
- High signal
- Could be due to
- High protein content
- High lipid content (triglycerides, No cholesterol)
- Can use fat suppression sq
- Rare intralesional hemorrhage can also result in intrinsic high signal
- T1 C+ (Gd)
- Thin enhancement around the periphery may sometimes be seen
- In the rare cases of malignant degeneration, enhancement becomes more pronounced
- T2
- Isointense to CSF: 65%
- Slightly hyperintense: 35%
- Hypointense: Rare
- Usually in the setting of the so-called white epidermoid (the term refers to the T1 appearance)
- FLAIR
- Often heterogeneous/dirty signal
- Higher than CSF
- Beware of flow artefact from CSF pulsation which can mimic this appearance
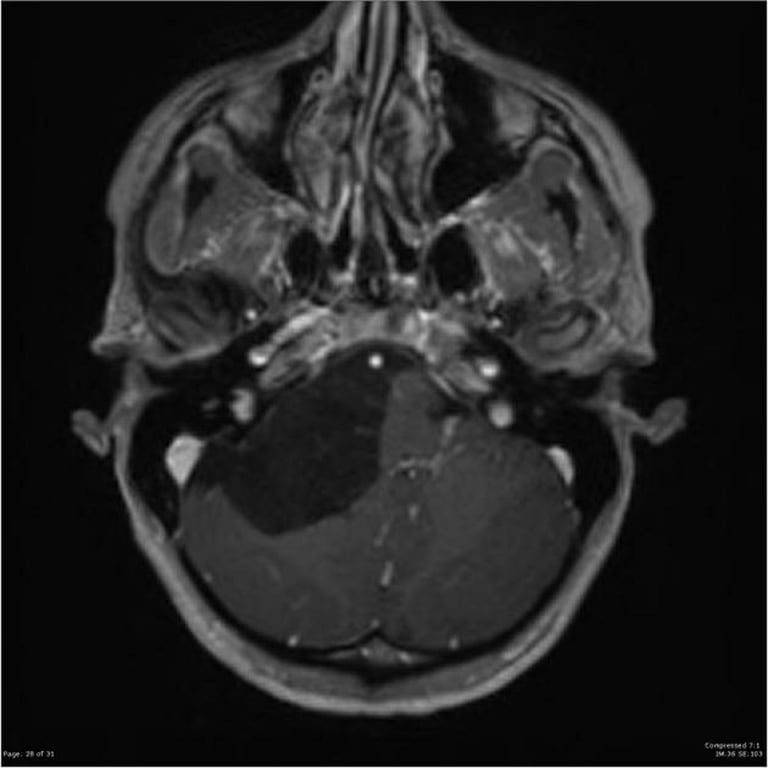
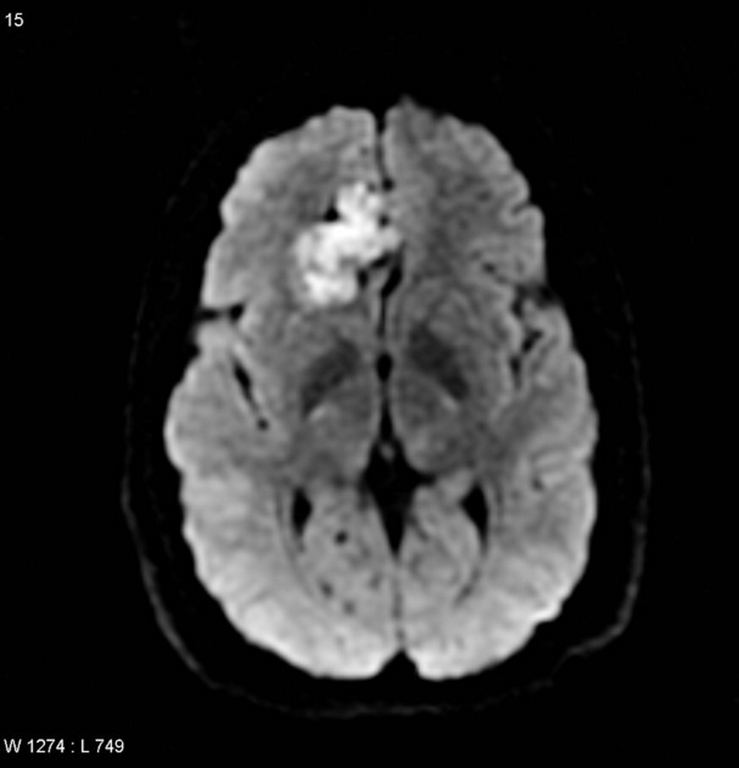
- DWI
- Useful for differentiation from arachnoid cysts
- Arachnoid cyst shows T2 shine through
- Epidermoid cyst shows restriction (T2 and ADC hyper intense) but unlike abscess or highly dense tumour it shows a ISOINTENSE ADC map
Images


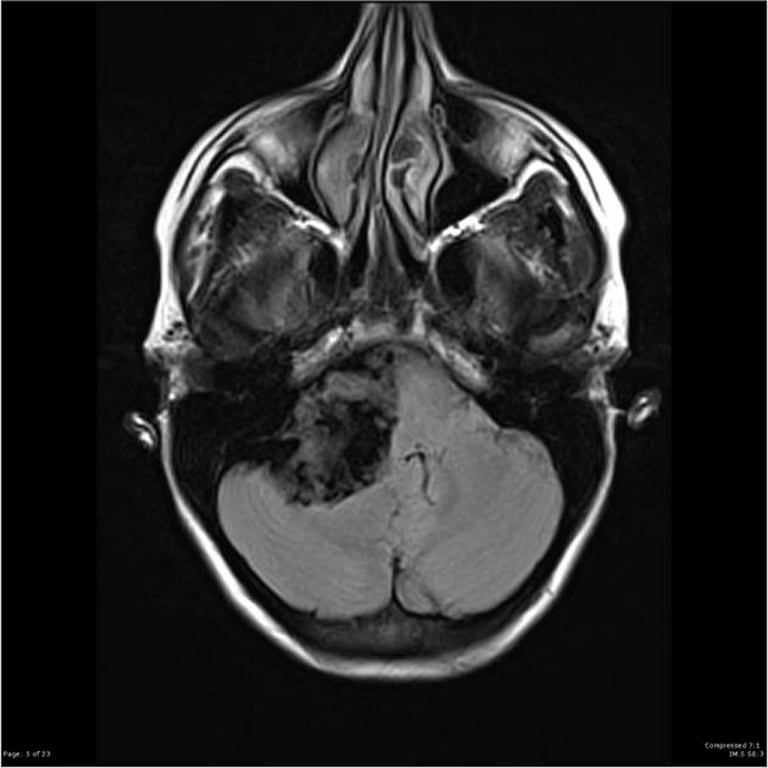
T1
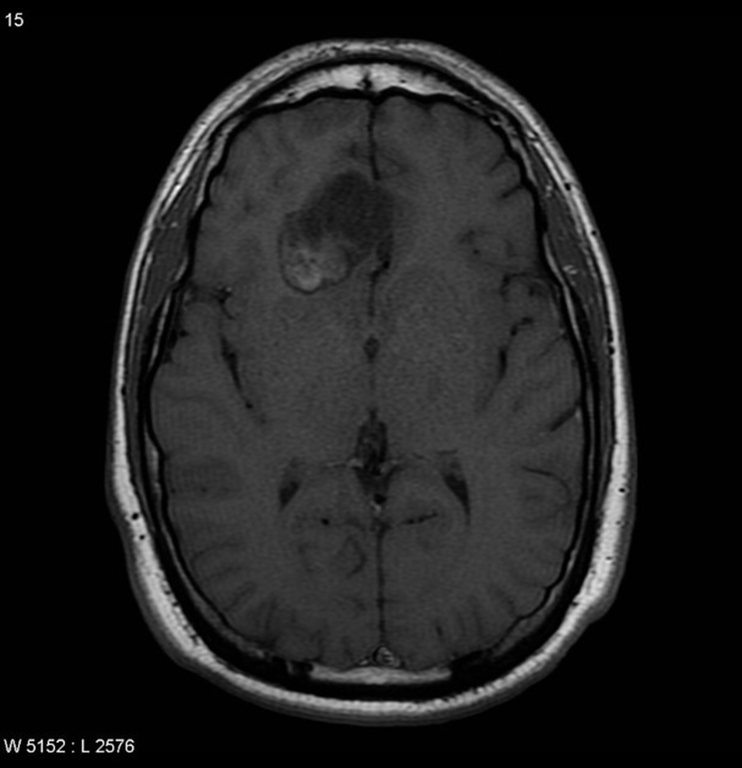
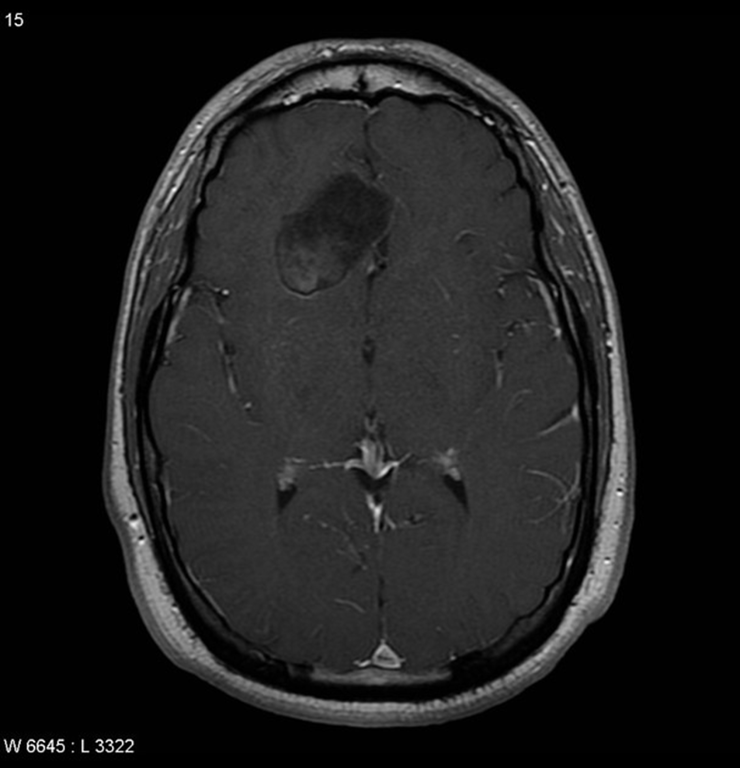
T1+C
T2
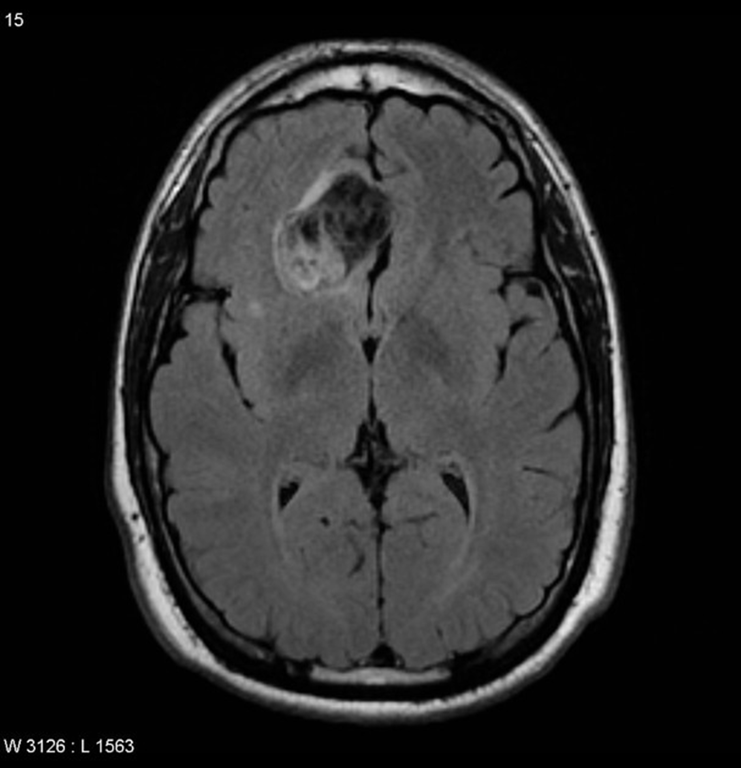
FLAIR
DWI


ADC
SWI

FIESTA

Histopathology
- Macroscopic
- White and pearly,
- Can be smooth, lobulated, or nodular
- Contents: creamy, waxy material

- Microscopic
- Cyst Wall are lined by
- Stratified squamous epithelium, and
- Contain
- Keratin (from desquamated epithelium)
- Cellular debris
- Cholesterol
- Cyst contents:
- Liquid or
- Flaky consistency.
- Growth occurs at a linear rate like normal skin,
- Unlike the exponential growth of true neoplasms
- They tend to spread along normal cleavage planes and surround vital structures (cranial nerves, ICA…)
- Bony destruction
- Minority
- Usually occurs with larger tumors
- Rare malignant transformation → squamous cell cancer
- In cases of repeated recurrences after multiple surgeries.
Treatment
- Surgery
- Curative
- Symptoms are from mass effect
- An STR to preserve neurological function is preferable to GTR if neurological morbidity is high
- Cyst spillage of fat droplets causes chemical meningitis
- Minimize spilling → may cause severe chemical meningitis (Mollaret’s meningitis, see above).
- To reduce chemical meningitis
- Intraoperative irrigation with hydrocortisone (100mg/L of LR) to reduce the risk of post-op communicating hydrocephalus.
- Perioperative IV steroids and copious saline irrigation during surgery may provide similar results.
- Recurrence
- Mean 12 years from 1st resection
- The tumor is not in the cyst wall → remove as much as possible but to leave capsule adherent to critical structures such as brainstem and blood vessels because
- As the morbidity of removal is high
- A small residual does not preclude satisfactory outcome.
- In spite of adequate removal, it is not unusual to see persistent brainstem distortion on post-op imaging.
- Post-op radiation is not indicated as the tumor is benign and does not prevent recurrence
Differential diagnosis
Dermoid cyst
Features | Intracranial Epidermoid Cysts | Intracranial Dermoid Cysts |
Frequency | More common 0.5–1.5% of brain tumors | Rare 0.3% of brain tumors |
Location | Off midline (CP angle) | Midline |
Presentation | Later | Earlier |
Origin | Congenital (arising from ectodermal inclusion during neural tube closure) | Embryonic ectoderm trapped in the closing neural tube between the 5th to 6th weeks of gestation |
ㅤ | Acquired (post-surgical or post-traumatic implantation) | ㅤ |
Lining | Simple skin cells, devoid of cutaneous-type adnexal structures Stratified squamous epithelium | Stratified squamous epithelium, containing epidermal appendages (hair follicles, sweat glands, sebaceous glands) |
Contents | Keratin, cellular debris, cholesterol, occasional hair No dermal elements: | Same as epidermoid, plus hair and sebum Dermal elements: Hair follicles, sweat glands, sebaceous glands (secreting sebum) |
Rupture | Less common | More common |
Meningitis | May have recurrent aseptic meningitis, including mollarets meningitis | May have repeated bouts of bacterial meningitis |
Associated anomalies | Tend to be isolated lesions | Associated with other congenital anomalies in up to 50% of cases |
Imaging Appearance | Identical to the petrous apex and middle ear congenital cholesteatomas | Well-defined lobulated midline masses with low attenuation (fat density) on CT and high signal intensity on T1-weighted MR images |
CT | Hypodense, slightly greater than CSF | Hypodense, similar to CSF |
ㅤ | Bone erosion in 33% | Lobulated margins |
ㅤ | No enhancement | Fine linear strands |
ㅤ | No enhancement | |
T1W MRI | Isointense, same as CSF | Typically hyperintense, same as fat |
ㅤ | Occasionally hyperintense around periphery; | No enhancement |
ㅤ | No enhancement | |
T2W MRI | Isointense or hyperintense, same as CSF | Variable |
FLAIR | Variable | Variable |
DWI | Restricted diffusion, hyperintense to CSF | Restricted diffusion, hyperintense to CSF |
Fat Saturation Sequence | Unchanged | High signal drops out |
Local Findings | Insinuates between neurovascular structures | More mass effect |
ㅤ | ㅤ | Associated abnormalities (e.g., Klippel-Feil, dermal sinus tract) |
Enhancement After Contrast | Not specified in the provided information | Typically do not enhance |
Associated abnormalities | Absent | May be present |
Surgical resection | Difficult | Less difficult |
Cholesterol granuloma
Feature | Epidermoid | Cholesteatoma | Cholesterol granuloma |
Origin | Ectodermal cells in abnormal location (within CNS, intradural) | Ectodermal cells in abnormal location (within ear, extradural) | Chronic inflammatory cells surrounding cholesterol crystals (? from breakdown of RBC membranes) |
Precursor | Usually congenital, occasionally acquired, e.g. after LP (p. 1601) | Usually acquired (following chronic infection ? due to epithelial cells from tympanic membrane), occasionally | Chronic middle ear infection or idiopathic hemotympanum |
Symptoms | Vary depending on location | Congenital chronic hearing loss, ear drainage, pain, or numbness around ear | Usually involve vestibular or cochlear dysfunction |
Imaging (may not reliably distinguish among these) | CT: low density; no enhancement; bone erosion in only 33% MRI: TIWI: intensity slightly>CSF; T2Wl: tumor & CSF similar high intensity | CT: low density; no enhancement; bone erosion in only 33% MRI: TIWI: intensity slightly>CSF; T2Wl: tumor & CSF similar high intensity | CT: homogeneous & isodense; rim enhancement; extensive destruction of petrous bone MRI: increased signal on both TIWI and T2Wl |
Gross appearance | Pearly white | Pearly white | Brown (from hemosiderin) |
Microscopic pathology | Hyperkeratotic cyst lined with stratified squamous epithelium | Hyperkeratotic cyst lined with stratified squamous epithelium | Fibroblastic proliferation, hemosiderin-laden macrophages, cholesterol clefts, giant cell reaction |
Ideal treatment | Aggressive near-total excision | Aggressive near-total excision | Subtotal resection followed by drainage & restoration of pneumatization |
Adamantinomatous Craniopharyngioma
- Have similar histology
- Epidermoid cyst have
- Cholesterol components
- Keratin components
Arachnoid cyst
Characteristic | Arachnoid Cvst | Epidermoid |
CIS density | CSF | Slightly higher than CSF |
Margins | Smooth | Scalloped |
Calcification | No | 25% |
Blood vessel involvement | Deviates | Insinuates between vessels |
Intrathecal contrast | May take up but can be delayed | No uptake, defines borders |
Characteristic on MR sequence sensitive to CSF pulsation (steady state free precession) | Pulsates | Does not pulsate |
Diffusion | Dark | Bright |
ADC | Increased | Decreased |
FLAIR | Dark | Bright |