Number
- 20-30 years of age
- Male to Female ratio=1:3
- Hormonal changes play a part in their formation.
- Women get older the cyst initially enlarges and then shrinks.
- Males, they tend to remain stable over time.
- 1% of population
- Common
- Usual incidental
- 4% of MRI
- 25-40% of autopsies
- As many more are microscopic
Aetiology
- Obscure and may be due to ischemic glial degeneration or due to sequestration of the pineal diverticulum
Histology
- Cyst wall:
- Inner layer: finely fibrillary glial tissue often containing haemosiderin
- Middle layer: pineal parenchyma with or without calcification
- Outer layer: thin fibrous connective tissue
- Cyst contents:
- Proteinaceous fluid
- Clear
- Slightly xanthochromic → hemorrhagic fluid
Clinical Presentation
- Positional headache
- Cyst intermittently compress the vein of Galen and/or Sylvian aqueduct
- Still unproven
- Enlarge and causes compression 61
- Aqueductal compression → Hydrocephalus
- Tectal compression → gaze paresis
- Including Parinaud’s syndrome
- Hypothalamic symptoms
- Pineal apoplexy: Haemorrhage into a pineal cyst can cause rapid expansion
Progression
- Nonneoplastic, benign
- Adults: Risk of growing is ≈ 4% with 6 months median follow up
- PCs <2cm diameter with typical appearance (wall: ≤ 2mm thick and no irregularities or nodular enhancement): are generally considered not to grow, but the natural history is not known with certainty.
- Children: 11% in children with 10 months median follow-up
Imaging
- General
- Like the pineal gland, the walls of pineal cysts do not have a well-formed blood brain barrier → enhance vividly with contrast
- Well circumscribed fluid density lesions
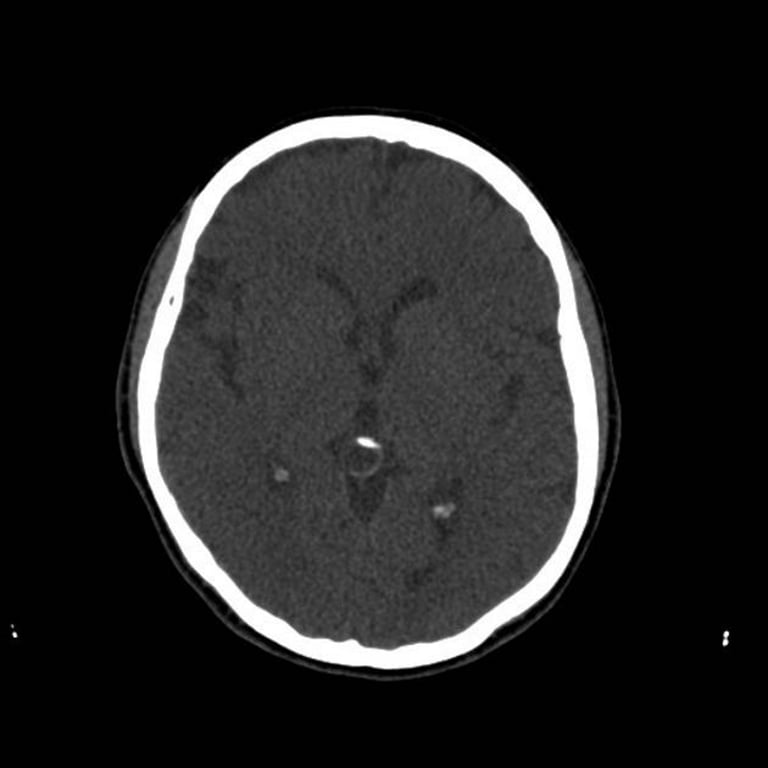
- Thin rim calcification seen in 25%.
- Thin, smooth peripheral enhancement is also often seen.
- The internal cerebral veins are elevated and splayed by the cyst.
- 15-20mm in size
- CT
- May not be seen due to cyst fluid density similar to CSF

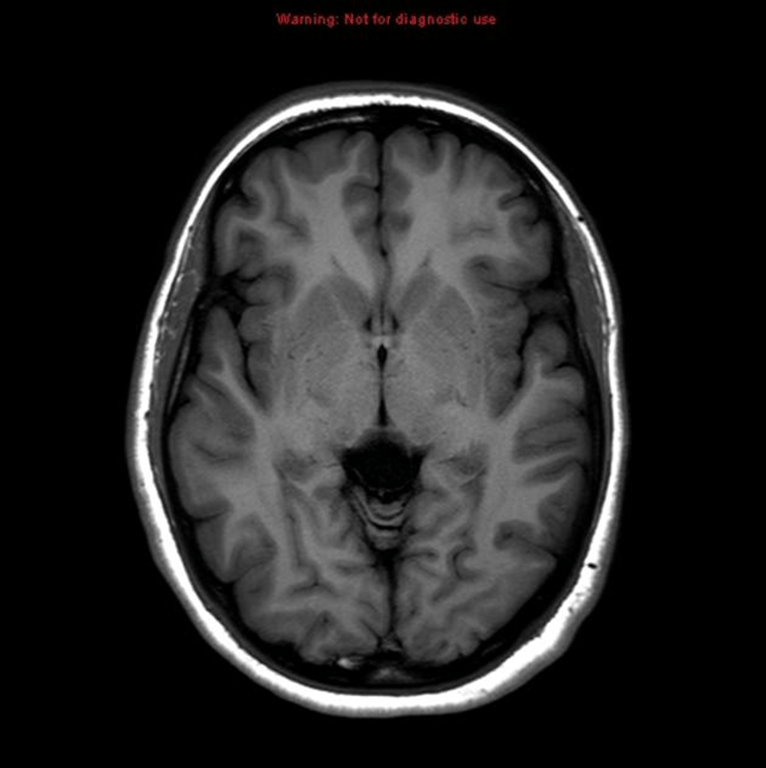
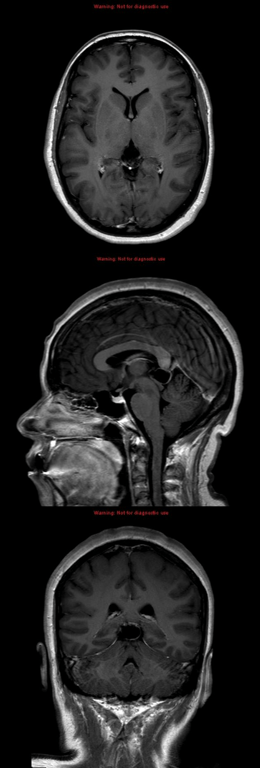
- MRI
- T1
- Typically iso/hypointense compared to brain parenchyma
- 55-60% hyperintense when compared to CSF
- Usually homogeneous in signal
- T1 C+ (Gd)
- 60% enhance
- Enhancement
- Usually thin (<2 mm)
- Smooth
- Confined to the rim (either complete or incomplete)
- If post-contrast imaging is delayed (60-90 min) gadolinium may diffuse into the cyst fluid and may lead to the mass appearing solid
- In atypical cases enhancement may be nodular, or there may be evidence of previous hemorrhage into the cysts
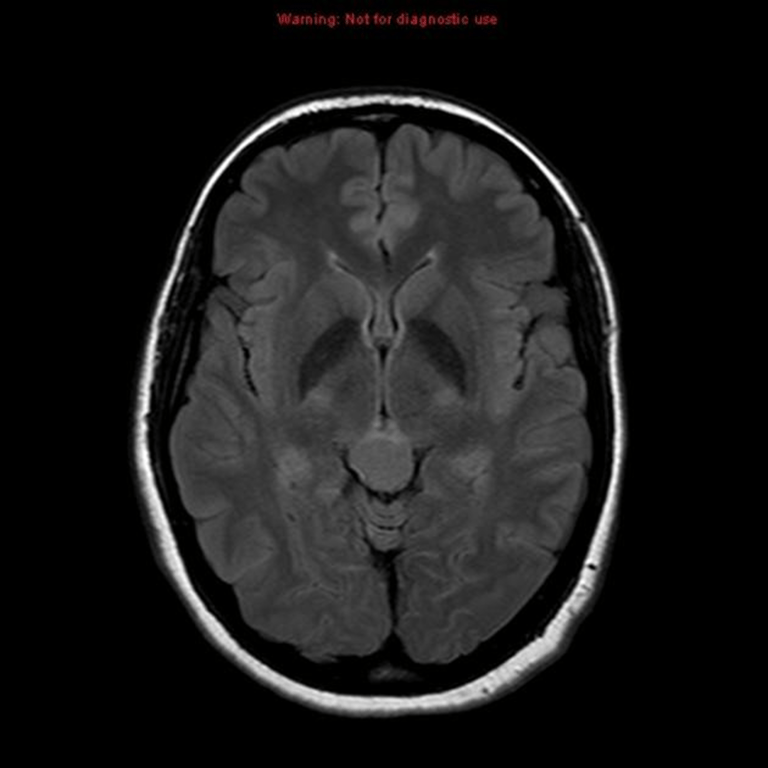
- T2
- High signal
- Usually slightly hypointense to CSF
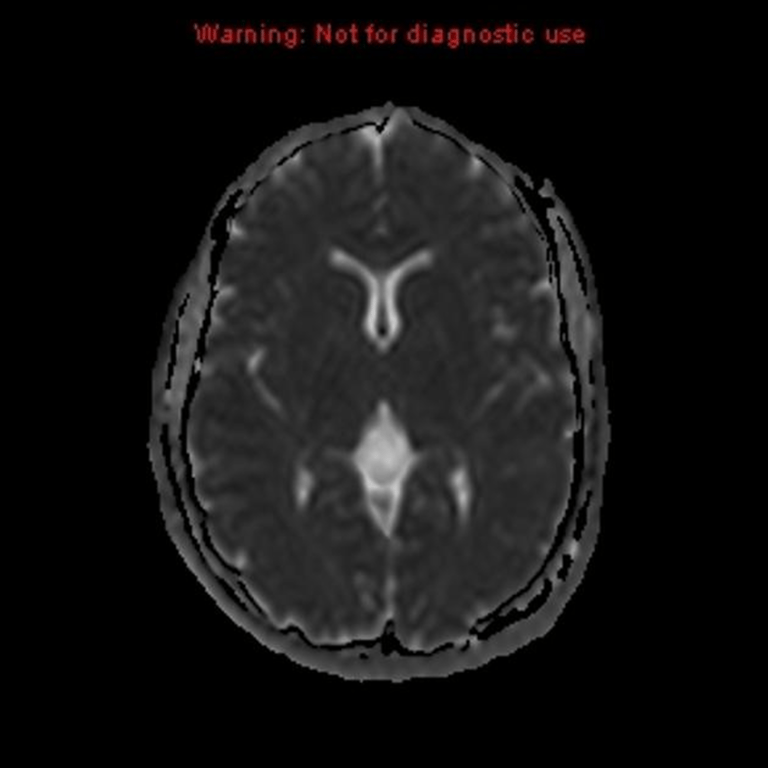
- FLAIR:
- High signal does not often suppress fully
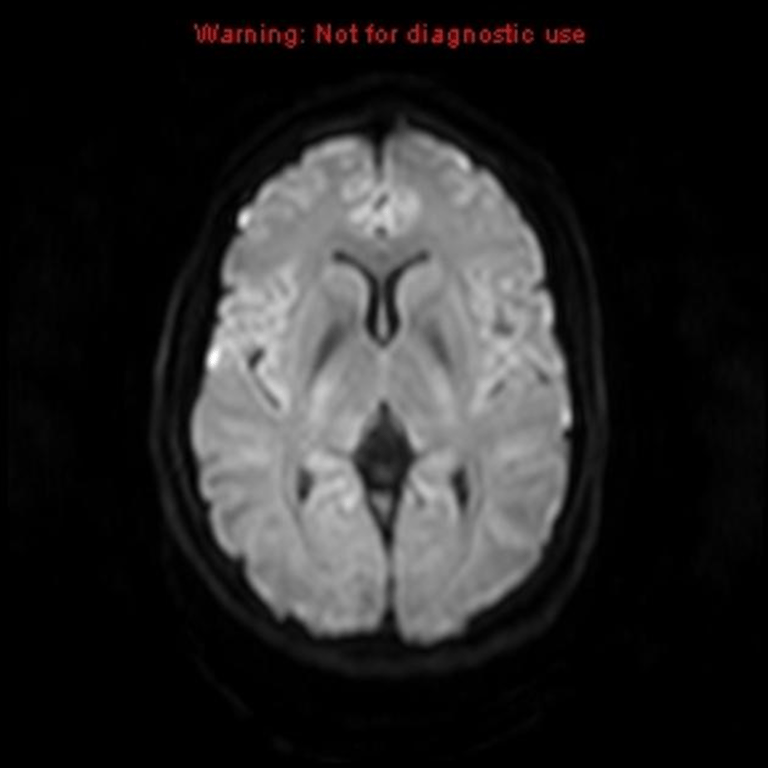
- DWI/ADC:
- They demonstrate no restricted diffusion
Images
T1
T1+C
T2
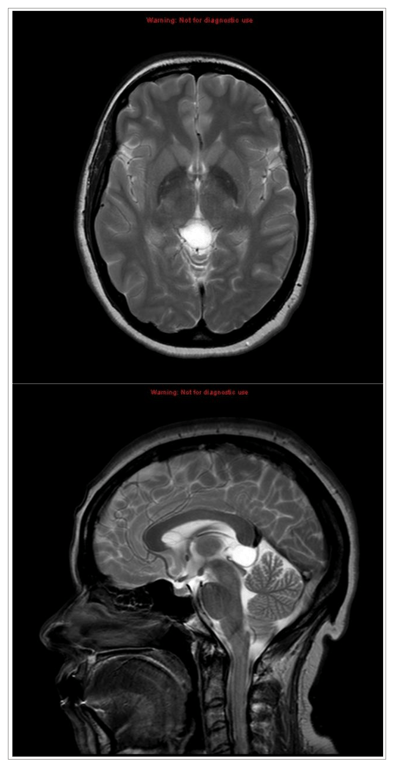
Flair
DWI
ADC
Treatment
- Asymptomatic:
- 1 yr follow-up MRI if stable then d/c
- If rapid growth do more fq scans
- Symptomatic lesions or those that show changes on MRI. Surgery to relieve symptoms and/or to obtain a diagnosis.
- Hydrocephalus.
- Surgical options include:
- CSF diversion:
- Recommended only for lesions with appearance to typical PC as it does not obtain tissue for pathology.
- May not relieve gaze disturbance from direct pressure on tectal plate
- Example:
- CSF shunt
- ETV
- Aspiration only (stereotactic or endoscopic):
- May not get enough tissue for diagnosis
- Cyst excision (open or endoscopic):
- Relieves symptoms
- Establishes diagnosis
- Low morbidity
Differential diagnosis
- Pineal parenchymal tumours
- Pineocytoma
- Pineal parenchymal tumour with intermediate differentiation
- Papillary tumour of the pineal region
- Epidermoid cyst
- Arachnoid cyst: these are usually posterior to the pineal gland
- Germ cell tumours:
- Germinoma
- Embryonal carcinoma
- Choriocarcinoma
- Teratoma
- Cerebral metastasis
- Vein of Galen aneurysm