General
- Aka: pars intermedia cyst
Definition
- Slow-growing nonneoplastic lesions that are thought to be remnants of Rathke’s pouch
- Same origin as
- Pituitary adenomas
- Adenohypophysis
Numbers
- Found incidentally in 13–23% of necropsies.
Origin
- Anterior wall of Rathke’s pouch
- RCCs and pituitary adenomas have a similar lineage and rarely they are found together
Pathology
- Rathke pouch forms during 4th week of embryonic development
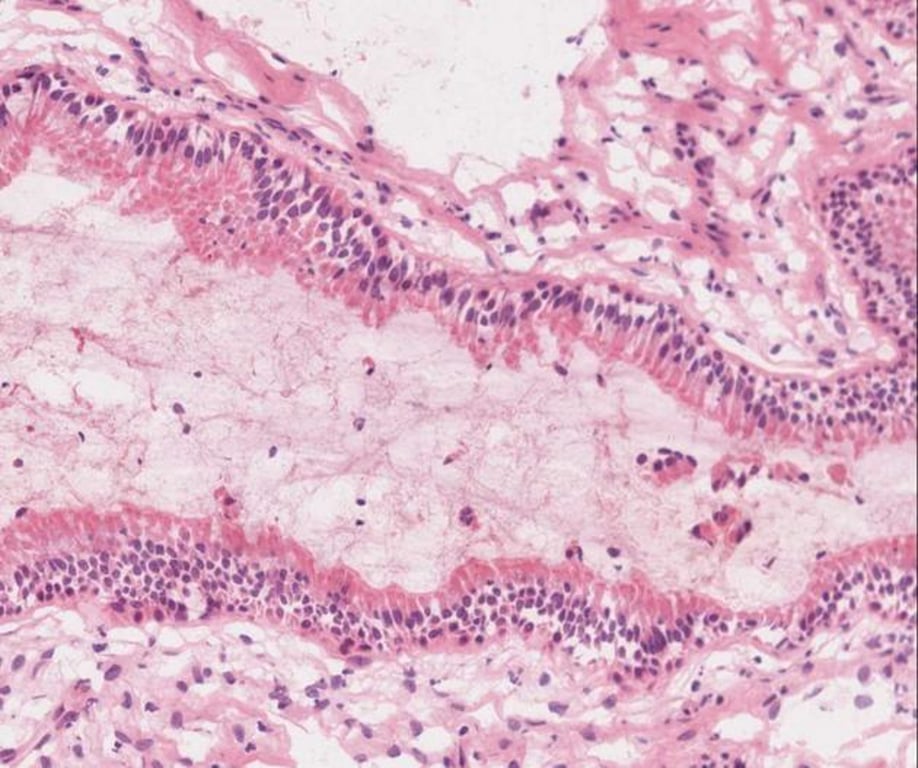
- Wall of cyst lined by a single layer of ciliated columnar epithelium with goblet cells
- Intraluminal nodule:
- Macroscopically appears white
- Adherent to cyst wall or free floating
- Consist of solid tissue made of desquamated cellular debris
Clinical presentation
- Due to mass effect and inflammation
- Most asymptomatic/incidental
- Headache
- 44-81% of symptomatic
- Sudden onset in 16%
- Endocrine disturbance
- 30-60%
- Males: Hypogonadism
- Fatigue
- Dec. libido
- Females:
- Premenopausal:
- Menstrual irregularities
- Galactorrhea
- Postmenopausal
- Panhypopituitarism
- Diabetes insipidus (37%)
- Visual disturbance (11-67%)
Imaging
General
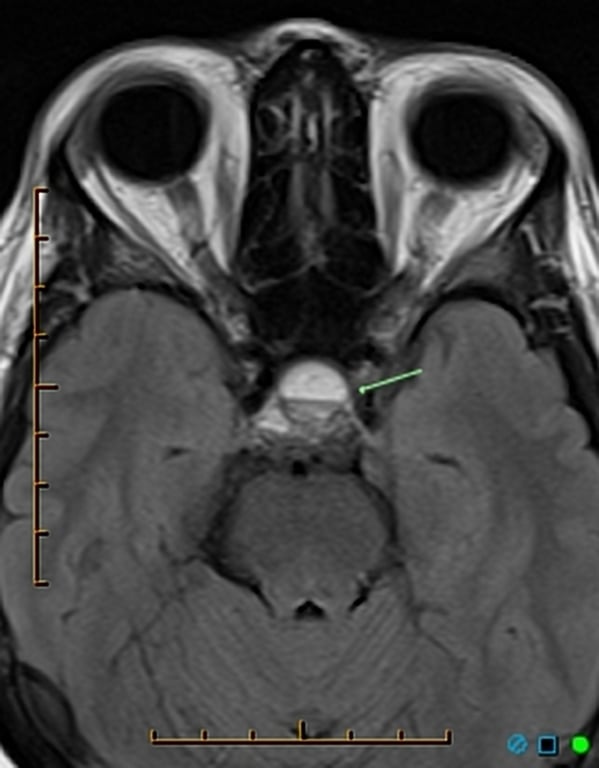
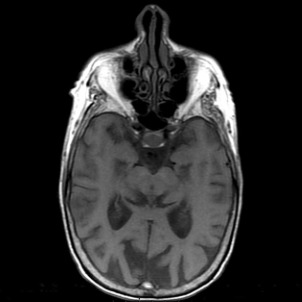
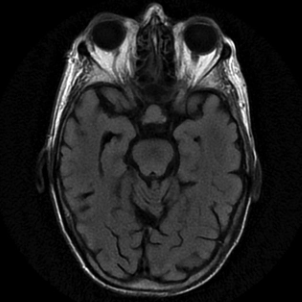
- Well defined non-enhancing midline cyst with in the sella between anterior and intermediate lobes
- 40% are intrasellar only
- 60% have supra-sellar component
- Midline without stalk deviation
CT
- Low-density cystic lesions.
- Infrequently can erode the skull base.
- CT+C: 50% capsular enhancement.


MRI
- Variable appearance
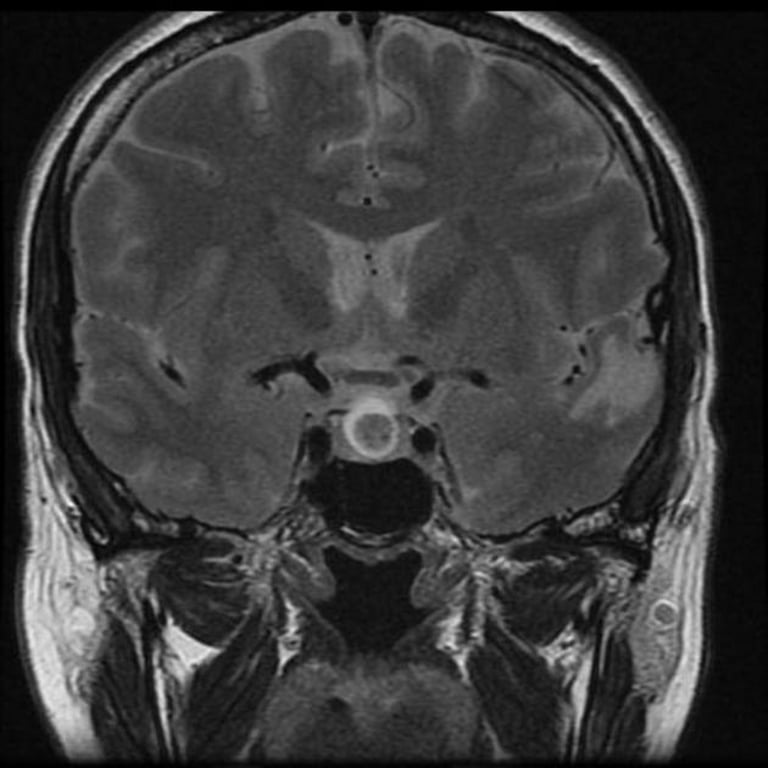
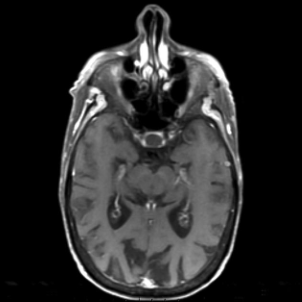
- T1
- Hyperintense
- 50%
- Proteinaceous mucinous contents
- Hypointense
- 50%
- Clear low protein fluid
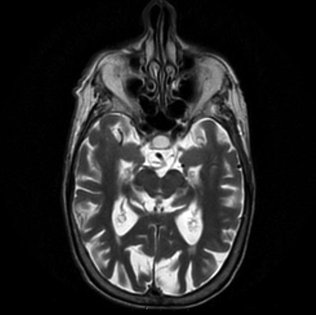
- T2
- 70% are hyperintense
- 30% are iso or hypo-intense
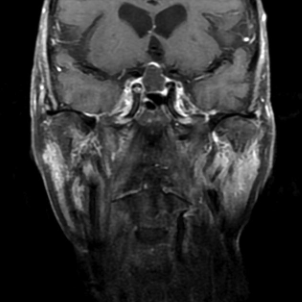
- T1+C
- No contrast enhancement of the cyst
- Thin enhancing rim of compressed pituitary tissue may be seen
- Intracystic nodule
- Pathognomonic for Rathke cleft cyst
- T1: hypertense
- T1+C: non enhancing
- T2: hypo-intense
- If a fluid level is seen = haemorrhage
Images
T1

T1+C
T2
FLAIR
Natural history
- 5% increased in size and 16% actually decreased in size with 27 months
- 69% showed no growth over 9 years
Treatment
- Incidental: f/u serial imaging
- Symptomatic: drained Transphenoidally (microscopically or endoscopically)
- Debate:
- Removing cyst wall have been said to reduce recurrence but has high incidence of post-op endocrine dysfunction
- No evidence of using H2O2 or Etoh irrigation to reduce recurrence rate
Outcome
Surgical
- Post-cyst decompression (Occur in 97% cases)
Improvements | Rates | ㅤ |
Visual disturbance | 83-97% | ㅤ |
Headache | 71% | ㅤ |
Endocrinopathies | 31-94% | ㅤ |
- Complications
- CSF leak
- 10%
- Higher rates with extension outside the sella
- Permanent diabetes insipidus (DI):
- Cyst drainage: 9%
- Cyst wall resection: 19–69%
Recurrence of cyst
- 16–18% over 2–5 years
- Higher if
- Purely suprasellar location,
- Inflammation and reactive metaplasia in the cyst wall,
- Cyst infection,
- Use of a fat graft within the cyst cavity
Differential diagnosis
Feature | Craniopharyngioma | Rathke’s cleft cyst |
Site of origin | Anterior superior margin of pituitary | Pars intermedia of pituitary |
Cell lining | Stratified squamous epithelium | Single layer cuboidal epithelium |
Cyst contents | Cholesterol crystals | May be clear or may resemble motor oil |
Surgical treatment | Total removal is the goal | Partial excision and drainage |
Cyst wall | Thick | Thin |