- Anatomy
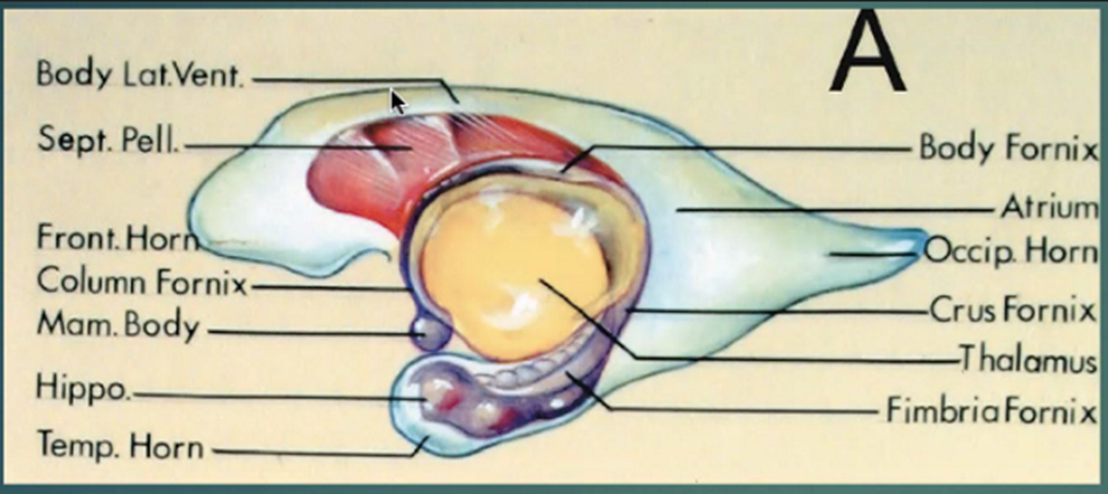
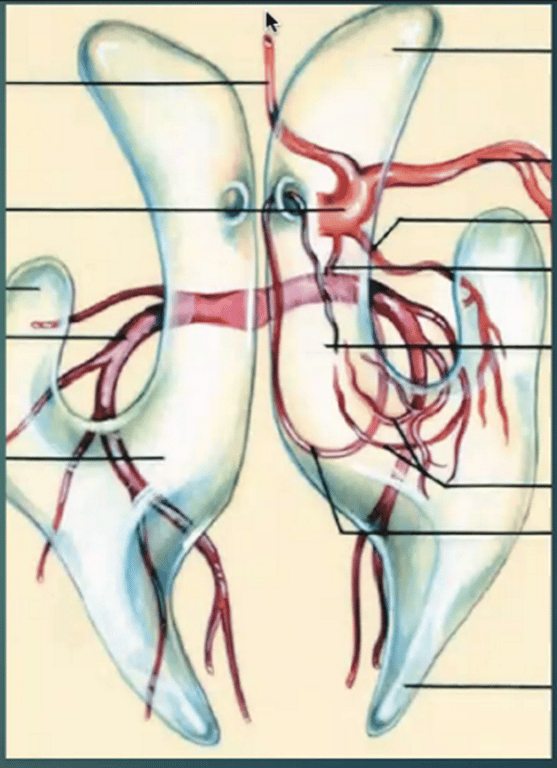
- See Ventricular anatomy
- Thalamus defines the different part of the lateral ventricles
- The mnemonic is “CENTRAL MS” for intraventricular lesion:
- C – Choroid plexus papilloma or carcinoma, colloid cyst, central neurocytoma, cavernoma
- E – Ependymoma, epidermoid/dermoid
- N – Neurocytoma
- T – Teratoma, tuber
- R – “Rule out” infection
- A – Astrocytoma, AVM, aneurysm, abscess, arachnoid cyst
- L – Lipoma, lymphoma
- M – Metastases, meningioma
- S – Subependymoma, subependymal giant cell astrocytoma
Numbers
- 1.2% of the primary brain tumours
Classification
Lateral ventricle
- Anterior body and frontal horn
- Ventricular walls (Most common)
- Septum pellucidum
- Central neurocytoma
- Primary septal tumours
- Rare
- Astrocytoma
- Lymphomas
- Germinoma
- Metastatic melanoma of the septum has been also reported
- Posterior body—trigone
Attachment | Cells of origin | Tumour | WHO grade | MRI features | Commonest location, associated conditions, pt population | CSF seeding, potential of recurrence |
Walls of the ventricle | Ependymal cells (glial cells with ependymal differentiation) | Ependymomas | 2,3 | Well defined, lobulated Heterogeneous calcifications, haemorrhage, cysts, TI Iso, T2 hyper, enhancement | Fourth ventricle if supratentorial can also be extraventricular, NF2 | Possible, can recur if not completely excised |
ㅤ | Subependymal glial cells | Subependymomas | 1 | Well defined, lobulated hyper@ T2, most are nonenhancing although some enhancement possible | Usually in the fourth ventricle, older pts than with ependymomas | Never, cured if completely excised |
ㅤ | Mixed neuronal and giant cell astrocytes within subependymal nodules in TS | Subependymal giant cell astrocytomas | 1 | Well circumscribed other subependymal nodules, TI Hypo-iso, T2 hyper, Avid enhancement | Lateral ventricle near the foramen of Monro, children with tuberous sclerosis | Never |
Septum pellucidum | Precursor neuronal cells | Central neurocytomas | 2,3 | Wide attachment on the septum pellucidum, well circumscribed, lobulated, can contain cysts, calcifications, rarely haemorrhages Iso@T1 Iso@T2, heterogeneous enhancement | Lateral ventricle near the foramen of Monro, young adults | Unlikely, can be cured if complete y excised, have higher recurrence rate higher recurrence if atypical |
ㅤ | Astrocytes | Astrocytomas | 2,3,4 | ㅤ | ㅤ | Unlikely, Likely to recur |
Trigone | Arachnoid cap cells within choroid plexus | Meningiomas | 1,2,3 | Lobulated, homogeneously enhancing | slightly more common on the left | Unlikely |
ㅤ | Choroid plexus | Choroid plexus tumours | 1,2,3 | Lobu ated avidly enhancing | Trigone, young adults | Rare for CPP I , II Frequent for CPC III. Whole spine MRI recommended |
ㅤ | Lymphocytes | Lymphomas | ㅤ | ㅤ | Rare | Unlikely |
Third ventricle
- Anterior third ventricle
- Foramen of Monro
- Colloid cysts are the commonest third ventricular tumours.
- Suprasellar tumours extending into the ventricles
- Craniopharyngioma (More common)
- Germinoma
- Optic pathway and hypothalamic gliomas
- Most often affects the paediatric population.
- Meningiomas from the skull base extending upwards.
- Posterior third ventricle
- Pineal region tumours
- Can grow into the posterior third ventricle.
- Meningiomas from the tentorial edge
- Arachnoid cysts
- Might be difficult to be spotted easily on first look.
- They can cause triventricular hydrocephalus.
- If they are symptomatic, they can be managed with endoscopic fenestration.
- Dermoid cysts—rare.
Attachment | Cells of origin | Tumour | WHO grade | MRI features | Commonest location, associated conditions, pt population | CSF seeding, potential of recurrence |
Foramen of Monro | Paraphysis elements from foramen of Monro | Colloid cyst | ㅤ | Hyper@T1 , iso/hypo@T2, no enhancement | Anterior third ventricle, foramen of Monro | Never, cured if completely excised, can recur if incompletely removed |
ㅤ | Choroid plexus | CPP, CPC | 1,2,3 | Hyper@TI , iso/hypo@T2, no enhancement | Rare | Rare for CPP 1 , 1 1. Frequent for CPC 11 1. Whole spine MRI recommended |
ㅤ | Arachnoid cap cells Vellum Interpositum | Meningiomas | 1,2,3 | ㅤ | Rare | Never |
Suprasellar | Squamous cells Rathke's cleft | Craniophangiomas | 1 | ㅤ | ㅤ | Unlikely, tend to recur if incompletely removed |
ㅤ | Germ cells | Germ cell tumours (germinomas and non-germinomas) | 3 | Isointense or slightly hyperintense for TI and T2 and homogenous enhancement | Pineal/suprasellar, children/young adults | Likely |
Posterior third ventricle | Intra-axial tumours from the thalamus can become exophytic into the posterior third ventricle, but most common y tumours in this area originate from the pineal region (see relevant chapter). Obstructive hydrocephalus is a usual initial presentation that needs to be treated as a first priority. | ㅤ | ㅤ | ㅤ | ㅤ | ㅤ |
4th ventricle
- Choroid plexus tumours
- Rare for this tumour in the fourth ventricle
- Exophytic brain stem gliomas
- Usually pontine gliomas.
- More common in children
- Cysticercosis
- Should be included in the differential diagnosis if the patient comes from or travelled in to endemic areas.
Attachment | Cells of origin | Tumour | WHO grade | MRI features | Commonest location, associated conditions, pt population | CSF seeding, potential of recurrence |
Walls/floor of the ventricle | Ependymal cells | Ependymomas | 2,3 | Well defined, lobulated, Heterogeneous +- calcifications, haemorrhage, cysts, Iso@T/, hyper@T2, enhancement | Fourth ventricle if supratentorial can also be extraventricular, NF2, | Possible, can recur if not completely excised |
ㅤ | Subependymal cells | Subependymomas | 2 | Well defined, lobulated hypo@T1 , hyper@ T2, most are nonenhancing although some enhancement possible | Usually in the fourth ventricle, older pts than with ependymomas | Never, cured if completely excised |
Symptoms
- Depends on their
- Location
- Tumours of the posterior third ventricle and pineal region
- Present with Parinaud’s syndrome
- Acute hydrocephalus
- Large posterior fossa tumours
- Acute obstructive hydrocephalus
- Depending on their size and extension with balance disturbance.
- Size
- Small tumours asymptomatic and found incidentally
- Large tumours in the left lateral ventricle can cause
- Memory disturbance
- Speech disturbance
- Motor deficit
- Epilepsy
- If they have a significant extraventricular extension into the parenchyma
- Visual disturbance
- Due to the direct pressure on the visual pathways
- Or from raised ICP
- Progress rate
- Rapid progression:
- Acute hydrocephalus (severe headache, drowsiness, nausea, and vomiting)
- Require CSF diversion before the definite management of the tumour.
- Slow growing tumours:
- Asymptomatic for a long time before they become symptomatic (usually present with a chronic, NPH-like clinical picture (cognitive decline, gait disturbance, and incontinence))
- Surgical management here can also address the resulted hydrocephalus
- The slow and gradual onset and progress of symptoms of low-grade tumours can rarely be accelerated by intratumoural haemorrhage, which leads to sudden deterioration
Differential diagnosis
- Depends on:
- Age of patient
- Location of tumour
- Clinical presentation
- Assocaited medical condition
- SEGA: tuberous sclerosis
- Pattern of growth
- Confined in one ventricle or can extend into the adjacent ventricle (e.g. central neurocytoma)
- Grows into an adjacent cistern through outflow foramina (e.g. fourth ventricular ependymoma).
- Large tumours can extend through the ependymal wall out into the parenchyma (e.g. large meningiomas, or choroid plexus tumours)
- CSF and plasma tumour markers should be sent if germ cell tumours are suspected.
Radiology
- Whole craniospinal axis is indicated for tumours with known potential of CSF dissemination
Management
- Conservative
- Conservative management with serial imaging follow-up
- Indicated
- If the patient is asymptomatic
- Tumour is not growing
- Patient is not fit for surgery
- CSF diversion
- Obstructive hydrocephalus with deteriorating neurological state
- CSF diversion should be done first
- If 3rd ventricular tumours + bilateral foramen of munro blockage
- Bilateral drainage of the ventricles
- Methods
- EVD
- ETV + endoscopic biopsy of the tumour (e.g. posterior third ventricle/pineal region tumours).
- Slow growing tumours with chronic hydrocephalus, the management of the tumours can take the priority.
- CSF diversion only
- Indicated
- For older and unfit patients
- Tumour is considered low grade with an indolent clinical course
- e.g. subependymoma of the fourth ventricle in older people
- VP shunt
- Surgery
Tables
ㅤ | Ependymoma | Subependymoma | Choroid Plexus Papilloma | Choroid Plexus Carcinoma |
Calcifications | Common punctuate foci of calcifications to large calcifications | Relatively common in 4th v tumors, but not lateral v tumors | Fairly common and may be scattered punctuate calcifications to extensive calcifications | Same as papilloma |
Cysts | Supratentorial > infratentorial | Small cysts can occur. | Some | Same as papilloma |
Enhancement | Variable and heterogeneous Soft tissue component usually intense | Mild & focal or absent, but may be intense particularly on MRI 4th v > lateral v | Intense Dilated feeding vessels | Intense MRI shows prominent flow voids and dilated feeding vessels |
TIWI | 4th v: heterogeneous isointense to GM Supratentorial: hypointense to isointense | Heterogeneous hypointense to isointense to WM | Hypointense to isointense to normal brain | Heterogeneous |
T2Wl | 4th v: heterogeneous Supratentorial: hyperintense to GM | Hyperintense to WM Heterogeneous | Variable Sl, flow voids | Heterogeneous More vasogenic edema than papilloma |
Other | 4th ventricular lesions commonly extend through foramen of Magendie &/or Luschka | Does not invade adjacent brain Most common nonenhancing lateral v mass Little surrounding parenchymal reaction or mass effect | Often associated with hydrocephalus May extend out to CP angle; rarely multifocal or extraventricular | Screen spine with MRI to exclude drop metastases FDG-avid |
Location | 4th supratentorial When supratentorial more commonly extraventricular | 4th V > lateral vs (commonly in the frontal horn/ body) | Lateral vs (more common in children) 4th v (more common in adults) | Same as CPP May more commonly involve/invade 3rd ventricle than cpp |
CT | Isodense to hypodense Occasionally hyperdense (may be higher grade) Heterogeneous | Hypodense to isodense Well-defined, lobulated Heterogeneous | Isodense to hyperdense No brain invasion May engulf glomus | More heterogeneous with necrosis and brain invasion |