Anatomy
Basic science
Stimulation of vagal afferents
- Desynchronisation of cortex EEG
- Thalamic blood flow changes
- Significant basic science background
E-102 pan-European study of VNS therapy in children
- Seizure frequency, predominant seizure type, no AED change during follow up
- Mechanism
- The signal travels up CN10 to the brain stem and spreads across the diencephalon and cerebral cortex leading to
- Stabilisation of EEG
- Modulation of extracellular excitatory neurotransmitter levels
- VNS can increase levels of GABA and Noradrenaline in the brain
- Vagus nerve
- A parasympathetic efferent nerve
- 80% is afferent sensory fibers → nucleus tractus solitarius → through the parabrachial nucleus and locus ceruleus into the forebrain regions linked to mood regulation such as
- Amygdala
- Hippocampus
- Hypothalamus
- Insular cortex
- Dorsal thalamus
- Orbitofrontal cortex
- Other important limbic regions
Indication
Treatment resistant epilepsy
- General
- Mainly a palliative procedure
- It is difficult to predict preoperatively who will obtain better seizure control,
- Indications:
- Multiple and bilateral independent foci
- Generalized epilepsy with diffuse epileptogenic abnormalities
- Refractory idiopathic generalized epilepsy
- Failed intracranial epilepsy surgery
- Contraindications to cranial epilepsy surgery
- Other options for tx resistant epilepsy
- Responsive Cortical Stimulation (e.g. Neuropace)
- DBS (e.g. STN, anterior thalamus) are also options.
Depression
- Improved quality of life even when seizures unchanged
- Significant improvement in mood and affect noted in post-hoc analyses of VNS studies
- VNS improves co-morbid depression and anxiety
- Indication
- It was approved by the FDA for the treatment of severe, recurrent unipolar and bipolar depression in July of 2005.
- The initial rationale for using VNS for the treatment of refractory depression resulted from mood improvements in epilepsy patients treated with VNS, irrespective of the presence or absence of beneficial effects on seizure frequency.
- VNS demonstrated steadily increasing improvement of depressive symptoms with full benefit after 6-12 months, sustained for up to 2 years.
- These studies reported response rates of 30-40% and remission rates of 15-17% after 3-24 months of treatment.
- VNS mech for antidepression
- A rapid increase in the concentration of the monoamines, which then enhance neuronal plasticity/neurogenesis in the hippocampus.
- Newborn cells could then functionally integrate and restore the disturbed corticolimbic networks in depressed patients, and may explain the therapeutic lag of VNS in the treatment of depression
Under studies
- Psychiatric disease:
- Vagal stimulation can lead to increase
- Verbal memory to help manage dementia
- Open label studies in Alzheimer's disease show promise
- Possibly attenuate decrease in MMSE
- VNS may decrease pathological depolarisations
- Does VNS attenuate neuroinflammation?
- Is there a role in other neurodegenerative conditions?
- Early studies on Parkinson's disease underway
- Social cognition to help manage autism
- Chronic inflammatory disease
- Early trials on
- Rheumatoid Arthritis,
- Inflammatory Bowel Disease underway
- Mechanism: Cholinergic anti-inflammatory pathway
- Neural mechanism that inhibits proinflammatory cytokine release
- Acetylcholine of Vagal origin binds cholinergic receptors on macrophages → TNF and IL-I production inhibited
- VNS can recapitulate or augment this
- Influences on systemic and neural inflammation
- Primary headache disorders
- Mech
- VNS attenuates of pathological electrical activity
- Electrical phenomena including Cortical Spreading Depressions may underlie migraine
- Evidence
- Transcutaneous VNS improves migraine
- NICE Medical Technologies Guidance [MTG46] encourages VNS in cluster headache
- Acute brain injury and stroke
- VNS in Stroke and TBI - 1
- Prevention of secondary injury
- Anti-glutamate effect
- Pathological depolarization perpetuate secondary injury in TBI, stroke, aSAH, neuroinflammation via Glutamate meditated excitotoxicity
- VNS attenuates spreading depolarisations (threshold and rate)
- Anti-inflammatory
- Upregulates central adrenergic pathways
- Decreases ICP in animal studies
- 30-40% reduction in infarct volumes in experimental MCA occlusion
- VNS in Stroke and TBI - 2
- Promoting neurorehabilitation
- Upregulation of Neuroplasticity
- Mobilisation of endogenous neural stem cells
- Randomised human studies of Physio + VNS following stroke show promising improvement in limb power and function
Technique
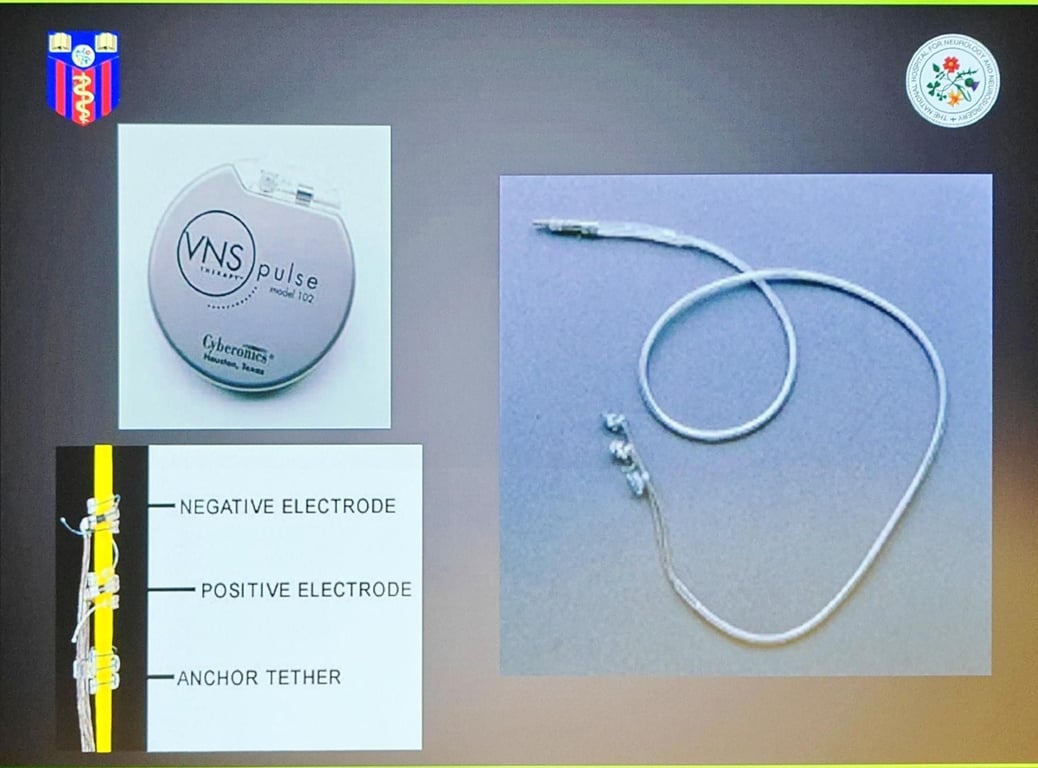
- 2 types
- Implanted
- Transcutaneous
- Applied to neck
- Vagal auricular branches
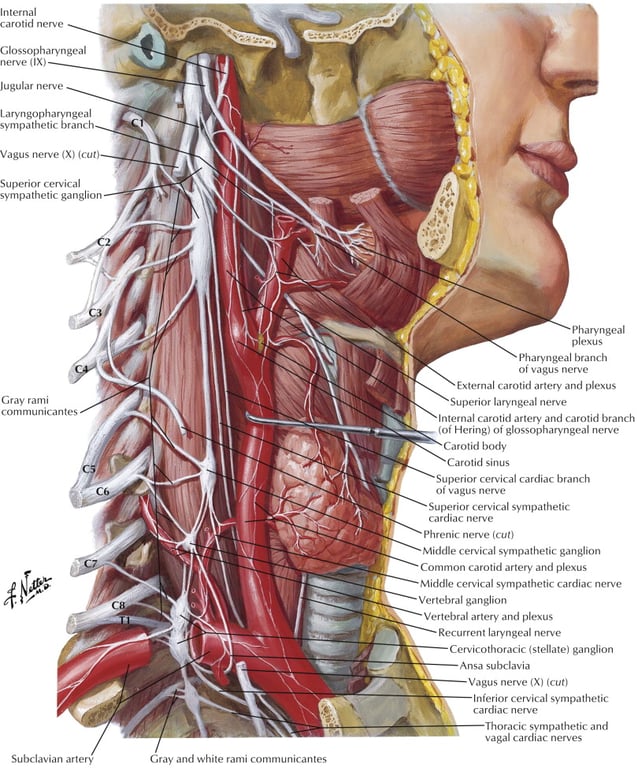
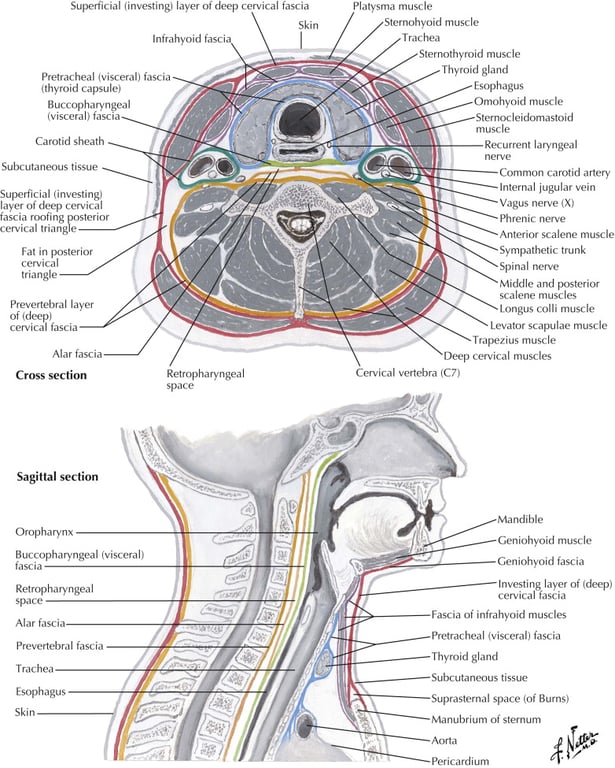
- Positioning
- Prone, with the left shoulder abducted to expose the pectoral region.
- Head should be tilted to the right to expose the left side of the neck.
- Use left vagal nerve as it has less cardiac supply
- Anterior chest incision is made and dissection down to pre-pectoral to create a pocket.
- A transverse neck incision is made in a skin crease over sternocleidomastoid (SCM) ⅔ of the way from jaw to clavicle.
- Platysma is split to expose SCM.
- Dissection down the medial border of SCM will expose the carotid sheath beneath.
- Open the carotid sheath to reveal (medial to lateral)
- Common carotid
- Vagus
- Jugular
- A 3cm length of vagus nerve is dissected free and rubber slings passed under it.
- The wire is tunnelled as per a shunt.
- The coils are wrapped around the vagus nerve with minimal trauma. Stimulator pack buried in pectoral pocket.
- Post op
- The VNS output is gradually ramped up at approximately 2-week intervals over a period of several months.
- Typically, a few months are required before efficacy of the VNS for a particular patient will become evident.
- The VNS generator typically has enough energy to last 3-5 years, depending on the settings and the amount of magnet usage.
Complications
- Hoarseness,
- Due to
- Surgical manipulation of the recurrent laryngeal nerve or
- Current spread during stimulation,
- Reported in > 30% of patients
- Some children experience a mild cough or hoarse voice during the first day after the VNS is ramped up, but they quickly adapt to this.
- Hypersalivation
- Contraindication to MRI.
- All old stimulators are MRI incompatible
- Risk of thermal injury to the vagus nerve.
- Thus, all patients should ideally have a relatively recent MRI before the VNS is implanted.
- The VNS is relatively contraindicated in patients with tumors that will require serial imaging, such as children with tuberous sclerosis.
- Newer stimulators are MRI conditional
- Criteria
- 1.5T MRI only
- Before scheduling an MRI, VNS device should be temporarily turn off
- After the MRI, Turn the VNS device back on
- Most common risks being
- Bleeding
- Infection
- Nerve injury.
- Fracture in the lead
- Is suggested when
- A previously effective VNS loses efficacy,
- Adequate generator energy is present, and
- The DC current is high when the VNS is interrogated.
- Occasionally can be seen on a plain X-ray
- Management
- Removal of the lead and its replacement should only be considered for those children who have demonstrated a significant improvement in their quality of life, because the risks of bleeding and nerve injury are much higher than with the initial surgery.
Notes
- When a child undergoes other surgical procedures with anaesthesia, it is generally recommended that VNS output current be set to zero with the programmer.
- In emergencies the magnet can be taped over the generator.
- Families need to be counselled to advise their other health care providers of the need to reprogram the VNS so arrangements can be made.
Outcome
- Seizure control itself is not the great
- 1/3 have significant improvement in seizure frequency,
- <5% of patients are rendered seizure free,
- 1/3 have mild to moderate improvement
- 1/3 have no benefit.
- 50% reduction in seizure frequency in approximately 2/3 of children
- Seizure frequency may not decrease overall it may become short enough to avoid emergency measures, or reduce the impact at school.