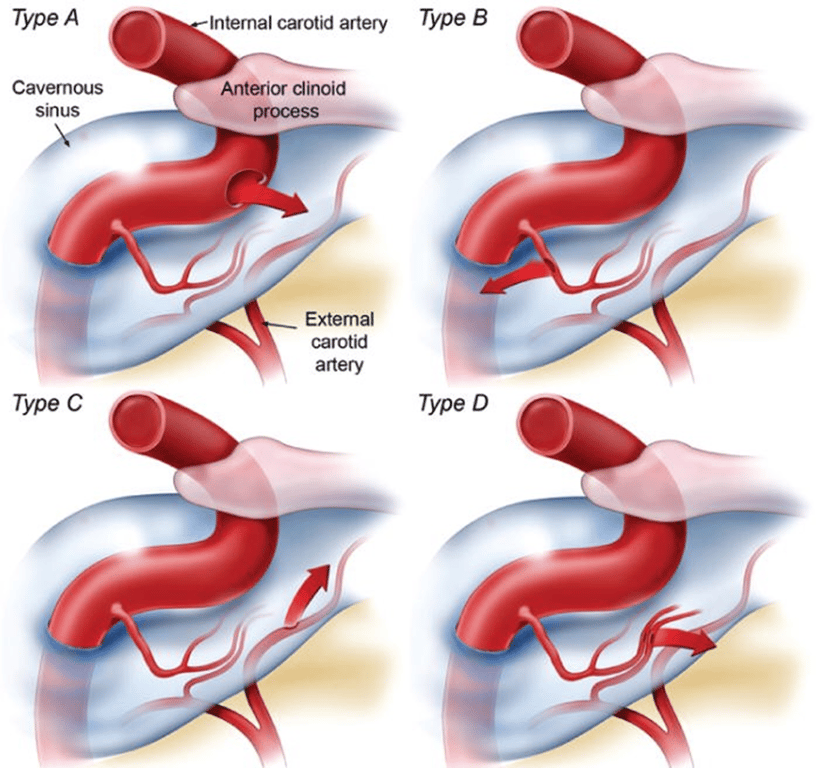
Classification
- Barrow classification 1985
Direct | Type A | Direct high flow shunts between InternalCA → cavernous sinus ~Traumatic ~Iatrogenic: trigeminal rhizotomy, Endovascular procedure ~Spontaneous: rupture of ICA aneurysm |
Indirect | Type B | Low flow shunts from meningeal branches (a dural artery branch of InternalCA) → cavernous sinus |
Indirect | Type C | Low flow shunts from meningeal branches (a dural artery branch of ExternalCA) → cavernous sinus |
Indirect | Type D | Low flow shunts from meningeal branches (a dural artery branch of both InternalCA and ExternalCA) → cavernous sinus |
Presentation (indirect have more gradual onset than direct): TRIAD for DIRECT: exophthalmos + chemosis + visual loss
- Increased intracavernous pressure
- Orbital and retro orbital pain
- Chemosis: arterialisation of conjunctiva
- Dec. Visual acuity/neovascularization of iris or retina: venous ischaemia —> hypoxia retinopathy—> neovascularization
- Diplopia/pupillary dilation/Opthalmoplegia: venous engorgement of the orbital contents —> ischaemic compression of CN
- Inc. intraocular pressure: increased back pressure as venous drainage is affected. Initially unilateral but can progress to bilateral
- Transmitted arterial pulse to eye
- pulsatile proptosis
- Ocular/cranial bruit: High flow (type A) —> turbulent
- Rare SAH 5%
Clinical features | Fq |
Bruits | 80% |
Proptosis | 72% |
Chemosis | 55% |
CN4 palsy | 49% |
Complete ophthalmoplegia | 24% |
Visual lost | 18% |
Radiology
- CT/MRI demonstrates
- proptosis,
- serpiginous and engorged intraocular vessels including superior ophthalmic vein (seen on T2 to diff from rectus muscles)
- Convexity of lateral wall of cavernous sinus.
- Angiography:
- Shunt of blood from ICA into cavernous sinus —> rapid pacification of petrosal sinus/ ophthalmic veins
- Manoeuvres to slow blood flow and slow down filling the shunting arteries
- Huber: inject contrast up VA and press on affected carotid
- Mehringer-hieshima: inject contrast up ICA and press ICA below catheter
Treatment
- Low flow (indirect) CCF 20-50% spontaneously thrombose
- Observe --> As long as vision is stable and intraocular pressure is not raised
- 10 sec for every hour ICA compression
- Symptomatic high flow CCF don’t resolve spontaneously and best to tx ASAP
- Indications
- Elevated intraocular pressure >20mmHg
- Inc. filling of cortical veins on angiography —> can cause neurology due to back pressure like cognard type 2b to 5
- Proptosis
- Visual loss
- CN4 palsy
- Intractable bruits
- Endovascular tx
- Options
- Electrolytically detachable coils
- Amplatzer vascular plug
- Route
- Transarterial
- Always to go transarterial if the vessel is large enough.
- If it is Type B you can embolize the feeder artery with coils
- Otherwise you have to embolize the whole cavernous sinus
- Destructive option (Last option)
- carotid artery occlusion on either side of fistula provided that the patient can tolerate this after occlusion test.
- Distal occlusion must be done proximal to ophthalmic artery
- Occlusion test can be false positive where after occlusion, while the fistula is still open, blood can be stolen by fistula —> reduce cerebral blood flow —> neurological symptoms
- Transvenous:
- better for indirect CCF because
- small arterial feeders of indirect are small and hard to get to
- if you just embolize the arterial feeders and you can't ensure that the small feeders have collaterals.
- heart —> jugular —> petrosal sinus —> cavernous sinus
- Lower success than transarterial route
- Heart —> jugular —> supra-optic vein —> superior ophthalmic vein —> cavernous sinus
- Best to wait for a while to allow for arterialisation of veins so that they have thicker wall and wont be so fragile —> can rupture