Definition
- A disease of the vein/sinus where AV shunt is contained within leaflets of dura mater
- Exclusively supplied by branches of
- Carotid arteries or
- Vertebral arteries
Aetiology
- Acquired
- venous thrombosis
- In patients with acquired or genetically determined prothrombotic disorders
- prothrombotic states constitute no more than 30% of cases of DAVF
- Congenital (e.g. some types of vein of Galen aneurysms
Location usually adjacent to dural venous sinuses
- Transverse (lateral) Sinus
- Most common
- Slight left side predominance (65%)
- With the epicentre almost always at junction of transverse and sigmoid sinus
- Supplied by the post. Meningeal branch of the vertebral artery
- Tentorium
- Posterior cavernous sinus
- Supplied by the meningohypohyseal trunk
- Draining into transverse and sigmoid sinus
- Within 1 cm of the junction
Numbers:
- 10-15% of all intracranial AVM
- DAVF 1/3 rate of AVM
- Present between 40-50 yrs
- 60% female
- Rare in children but if forms will be bilateral
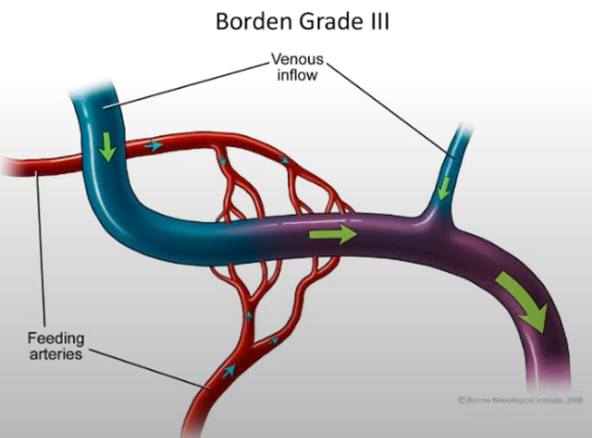
- Annual haemorrhage rate for Borden 2 and 3
- 20%
- Mortality 3%
Pathophysiology
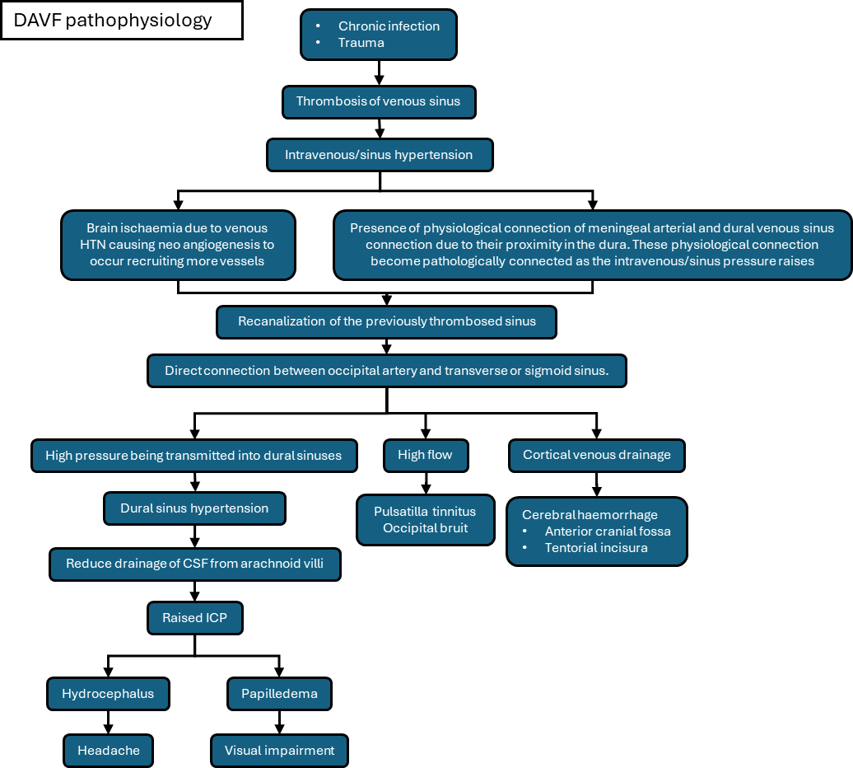
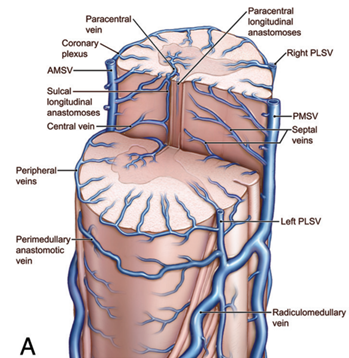
- one or more fistulae centred either
- Fistula on the bridging vein (bridging between the leptomeningeal veins and dural venous sinus)
- fistulae within the wall of veins contained within dura (including dural venous sinuses).
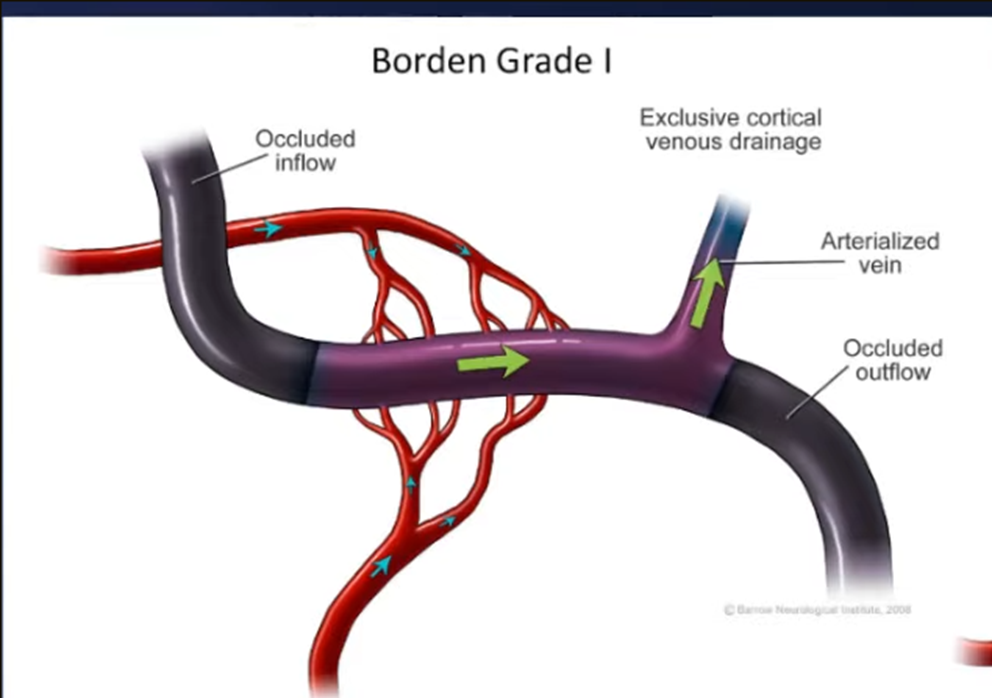
- No cortical venous HTN: low bleeding risk
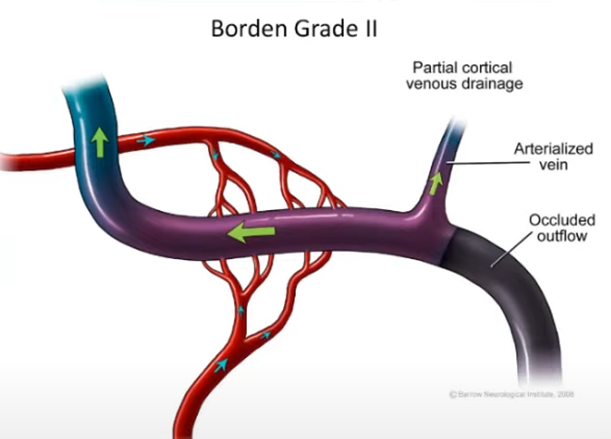
- Cortical venous hypertension/drainage: will have high bleeding risk
- Zipfel 2009
- haemorrhage risk
- Symptomatic (cortical venous HTN present) 7.4-7.6%
- Asymptomatic (cortical venous HTN absent) 1.4-1.5%
- Haemorrhage
- Re-haemorrhage rate: 35% within the first 2 weeks of hospitalization
- See Cognard and Borden classification
- Complication
- Venous aneurysm
- Arterial aneurysm
Clinical findings
Sign/symptom | No. (%) |
pulsatile tinnitus | 25 (92%) |
occipital bruit | 24 (89%) |
headache | 11 (41%) |
visual impairment | 9 (33%) |
papilledema | 7 (26%) |
- Symptoms can change and need re-evaluation
Classification
Cognard Classification
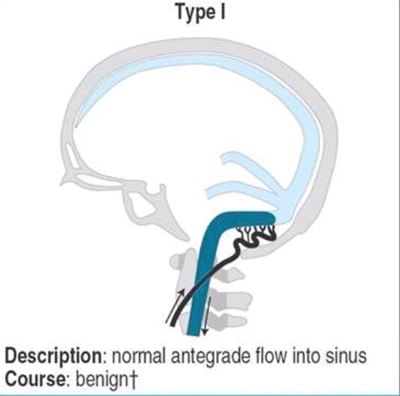
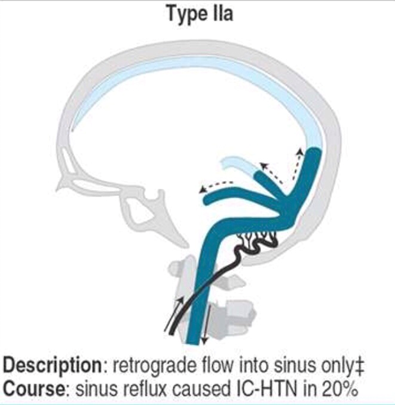
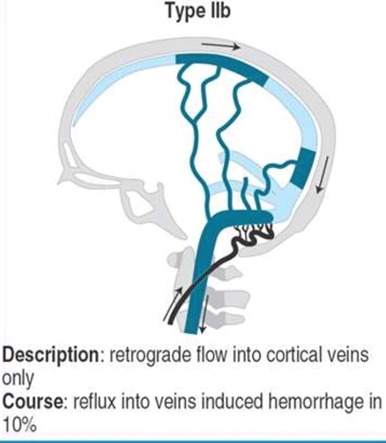
Type | Description | Notes | Annual risk of haemorrhage |
1 | Direct to sinus • Antegrade flow in sinus Anterograde drainage into the main sinus F/u for asymptomatic lesions: annual Doppler studies | Does not drain into cortical veins hence does not affect cerebral profusion —> MORE BENIGN Despite good prognosis 2% will progress —> require f/u studies | 0% |
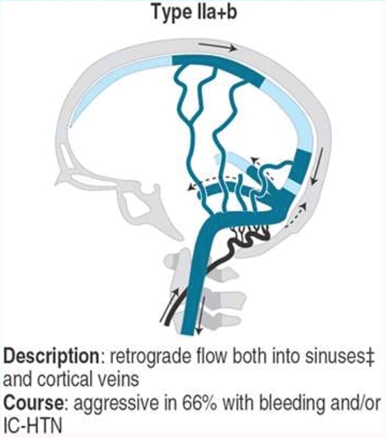
2a | Direct to sinus • Retrograde flow in sinus --> sinus can be non-functional but if other veins can help doing the drainage Blood is flowing in the wall of the venous sinus and not within the venous sinus Drainage into main sinus with reflux into another sinus F/u for asymptomatic lesions: annual Doppler studies Can cause raised ICP | As above —> MORE BENIGN | 10 |
2b | Direct to sinus • Retrograde flow into cortical veins | When cortical veins affected it can cause reduce drainage from normal cerebrum causing venous ischaemia in that region—> high risk of bleeding and intracranial hypertension | |
2a+b | Direct to sinus • Retrograde flow into sinus • Retrograde flow into cortical veins | As above | |
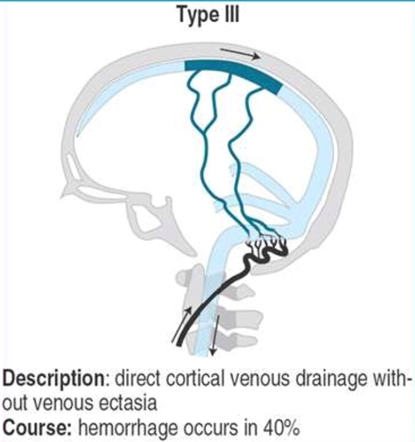
3 | Direct to cortical venous drainage • without venous ectasia Partial occlusion | 40 | |
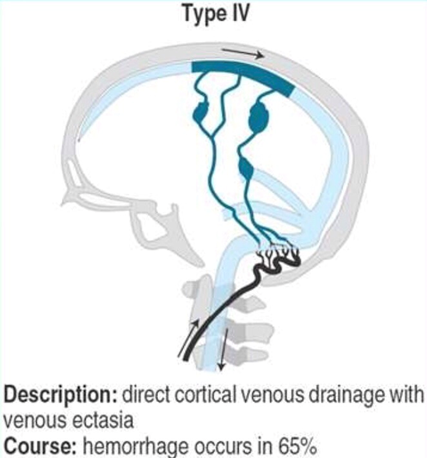
4 | Direct to cortical venous drainage • With venous ectasia ◦ dilatation of veins (>5mm and 3x larger than the diameter of the draining cortical vein) | 65 | |
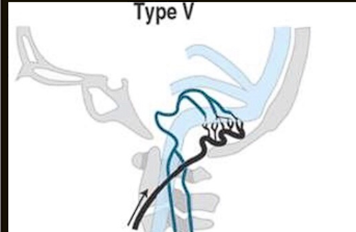
5 | Drainage into spinal perimedullary (a spinal) vein More likely to present with ischaemic than haemorrhagic Di Chiro Type 1 Barrow Intradural dorsal spinal AVF | Description: spinal venous drainage in addition to all of the above Course: progressive myelopathy in 50% |
Borden classification
Borden type | Features | Annual Risk of haemorrhage |
Type I: | Via meningeal artery → drains anterograde to the venous sinus | 0% |
Type II: | Via meningeal artery → drains anterograde to venous sinus and sinus drains retrograde to subarachnoid (cortical) veins | 6% |
Type III | Via meningeal artery → drains retrograde direct to subarachnoid (cortical) veins | 10% without venous ectasia 21% with venous ectasia |
Radiology
Non-contrast CT
- NAD
- Can see complications of high-grade fistulas,
- Haemorrhage
- White matter oedema from venous hypertension.
MRI
- Usually normal
- oedema
- suggesting back flow
- Engorgement of pial veins
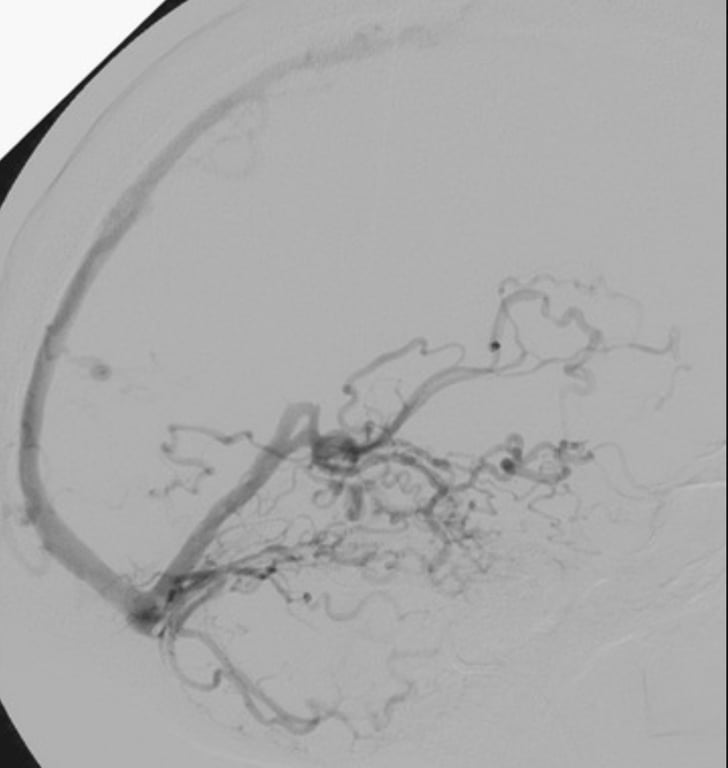
DSA
- test of choice
- Lateral angiogram of a Borden type III Right transverse sinus that was thrombosed distally. The catheter is situated in the proximal left transverse sinus, which has multifocal severe stenosis that functionally isolate the arterialized right transverse sinus pouch and force venous drainage retrograde. Contrast material refluxes into the superior sagittal sinus and supratentorial veins, as well as into the galenic system, occipital sinuses, and cerebellar veins
CTA
- Look for vessels penetrating the skull from the extracranial circulation that then feeds into the fistula at the dura venous sinuses.
Differential diagnosis
Features | AVM | DAVF |
Artery | Pial artery | Dural/meningeal artery |
Fistula | Parenchymal nidus Fistula located proximal to Bridging veins | Always at the dura Fistula located distal to Bridging veins |
Vein | Pial vein that eventually drains into a venous sinus | Always a venous sinus (There can be retrograde flow into the cortical veins) |
Management
- Aim
- Complete obliterate fistula (by closing the drainage)
- IF NOT ABLE TO
- At least downgrade it to reduce short term haemorrhage rates
- Strategy
- Identify and close the venous collector
- Functional channels in walls of sinus -superselective catheterization and balloon protection
- Non-functional sinus sacrifice
- Indicated for type 2B and below if
- Neurological dysfunction
- Haemorrhage
- Refractory symptoms
- Conservative
- Indication
- Lesions with a benign venous drainage pattern (Borden I or Cognard I/IIa)
- Due to low risk of haemorrhage or neurological deficit.
- Options
- Spontaneous regression of low-grade DAVFs, especially in fistulas involving the cavernous sinus.
- Manual carotid self-compression
- Rt hand Compress left carotid (so that if ischaemic the hand will drop off) —> reduce blood flow to the left side causes thrombosis of AVF
- Thrombosis rate 22%
- Clinical improvement rate 33%
- F/u clinically and radiographically, tof-MRA
- 1% to 3% chance of conversion from a benign to an aggressive drainage pattern.
- If symptoms change look for if there is an upgrade in grade
Intervention
- Indication
- Borden 2 and Cognard 2b and above
- Controversial
- (Borden I or Cognard I/IIa) incapacitating bruit, ocular symptoms, or headache, but this is quite controversial
- Complication
- Catheter entrapment
- Cranial nerve damage
- DMSO toxicity
- Radiation injury caused by prolonged fluoroscopic time.
Endovascular embolization
- 1st line
- Indication
- Sinus and/or cortical vein fistulation
- Onyx
- Properties
- Ethylene vinyl alcohol copolymer dissolved in dimethyl sulfoxide (DMSO)
- Onyx contains micronized tantalum powder
- After injection into the bloodstream, the DMSO leaves the mixture, causing the Onyx to precipitate without adhesion to the arterial lumen.
- Onyx solidifies within the vessel from outside to inside over several minutes, which allows it to be further pushed through the artery.
- Nonadhesive property that makes Onyx advantageous
- Decreases the risk of gluing in the catheter
- Allows the operator to more aggressively penetrate the fistula nidus.
- Can have reflux of onyx and can block an artery
- Especially true with skull base DAVF and facial nerve palsy
- Can see
- Artery into vein injection.
- Most AVF best tx endovascularly
- Options
- Transarterial embolization
- Most frequently used route
- microcatheter should be advanced to the distal arterial feeder, and the embolic material should be injected into both the fistula pouch and the proximal draining vein
- Outcome
- Rate of cure of 59% to 80% for malignant DAVF
- Complication
- permanent neurological: 0% to 3%.
- Transvenous embolization
- Before the widespread use of Onyx, transvenous embolization was considered the first-line endovascular treatment for DAVFs
- Technique
- Retrograde catheterization of the draining sinus or cortical vein AND
- Occlusion of the recipient venous pouch with coils, glue, or a combination of both
- involved sinus is often defunctionalized, which reduces the risk of concomitant venous infarction
- If the sinus still has some component of normal drainage, then embolization of the sinus should be avoided because it can lead to venous stroke and hemorrhage.
- Complication
- Vessel perforation
- Intracranial haemorrhage
- Venous infarction
- combined approaches
Microsurgery
- Indication
- Failed endovascular tx
- Esp: SSS and anterior fossa
- owing to the long distance that a microcatheter is required to travel to treat these lesions endovascularly
- Isolated cortical venous drainage not involving sinus
- Unfavourable physiological anastomoses
- Goal
- Disconnect the vein from the fistula point, which leads to a cure of the lesion
- Surgical options:
- Point-disconnection of cortical drainage
- Exposing the fistula with coagulation of direct arterial feeders as necessary
- Then the arterialized veins of the fistula are coagulated, clipped, or ligated in a location that is as close to the fistula point as possible, taking care to spare nonarterialized veins
- indocyanine green angiography and intraoperative digital subtraction angiography, when available, to confirm the obliteration of the fistula
- Isolation of sinus
- Packing of sinus channels
- Complication
- Heavy blood loss
- High blood flow into sinus —> inc. risk of bleeding if sinus is cut (8 units in 4 mins)
- Do not use craniotome
- Use a lot of dural tack up sutures
- From scalp, bone, dura, or fistula vessels themselves.
- Pre-op embolization can help reduce bleeding
SRS
- Used with or without embo
- Indication
- Reserved for benign DAVF that have failed other tx
- Salvage therapy for higher risk lesions that are felt to be too dangerous to approach endovascularly or surgically.
- Dose
- 20 Gy
- Cons
- Latency for which haemorrhage may occur
- 4 yrs delay before occlusion
- Complications
- Headache
- Nausea
- Delayed cyst formation.
- Outcome
- Cure rates ranging from 50% to 93%
- Higher cure rate in
- cavernous sinus DAVF
- SRS + Embolization
- Outcome
- Low grades (Cognac 1 or 2A) --> High grades
- 0.8-2%/yrs
- Tx DAVF
- 0.8-2%/yrs
