General
- Others: AVM, venous angiomas, cavernous malformations, mixed or unclassified angiomas
- A type of AOVM (angiographically occult vascular malformation)
Definition
- Aggregation of capillary-type dilated capillaries with normal intervening brain tissue that has low flow
- without smooth muscle or elastic fibres in their walls
- lined with a single benign endothelial cell layer
- If there is no intervening brain tissue it will cavernoma
Numbers
- 2nd most common vascular malformation affecting brain (1st AVM)
- Rare
- affecting ≈ 1 in 5,000 people
- Prevalence of 0.4-0.7 percent in the general population.
Histopathology
Macroscopic
- Capillary telangiectasias are small vascular lesions (mm to 20 mm) that do not exert mass effect.
Microscopic
- Capillary telangiectasias show localized aggregations of thin-walled dilated vessels without smooth muscle or elastic fibres, situated within brain parenchyma lacking adjacent gliosis or calcification.
Clinical presentation
- Incidentally found without clinical significance
- Risk of haemorrhage is very low, except possibly in brainstem
- Usually solitary, but may be multiple when seen as a part of a syndrome:
- Louis-Barr (ataxia telangiectasia)
- Myburn-Mason
- Sturge-Weber
- Brain capillary telangiectasia is not a part of hereditary haemorrhagic telangiectasia (HHT).
- HHT is an autosomal dominant neurocutaneous disorder characterized by mucocutaneous capillary telangiectasia and arteriovenous malformations and fistulae in lungs, liver, brain, and spine
Pathophysiology
- Capillary telangiectasias may be congenital due to failure of capillary involution or acquired via reactive angiogenesis from insults like irradiation or venous hypertension.
- Autosomal dominant
Location
- Pons: most common
- Can also affect the middle cerebellar peduncle, cerebral hemispheres, and spinal cord.
Imaging
- Usual multiple and incidentally found
- Can found together with Cavernomas
- CT
- Well demarcated homogeneous
- Mottled high density: due to bleeding, calcification
- A bit contrast enhancing
- Rare to have oedema or mass effect
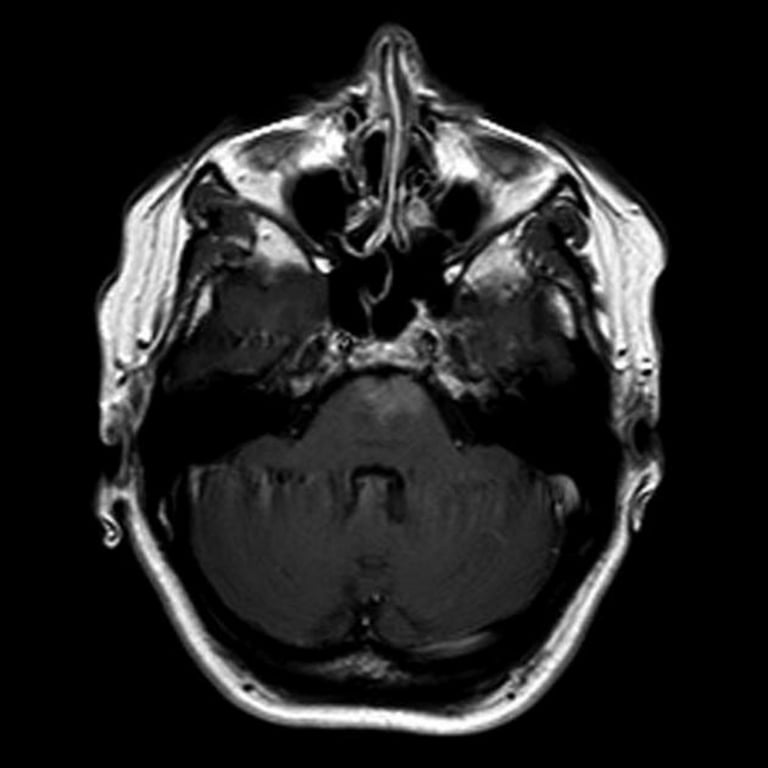
- MRI
- T1 C+: hyper intense
- T2:
- reticulated core of inc., and dec. intensity,
- if these was previous haemorrhage can have a rim of hemosiderin laden macrophages that comes up as hypointensity on T2
- SWI
- they can be seen as multiple hypointense foci.
Management
- Surgical indication:
- recurrent haemorrhage,
- medical intractable seizure
- SRS has not had a satisfactory high enough benefit to risk ratio