Vascular malformation that is part of venous drainage of the involved area with intervening brain present
- 0304526029 DVA + cavernoma
General
- Aka: Venous angiomas
- DVA are extreme variations of the normal venous system.
Numbers
- 0.43 (0.31–0.61) per 100 000 patients per year
- Most common out of all the vascular abnormalities
- 1/5 are combined CCM/DVA
- DVAs with three or more medullary veins in the same MRI section, infratentorial lesions, and multiple DVAs were more likely to be associated with a CCM
- Most common vascular malformation found in autopsy
Clinical features
- Usually asymptomatic
- Seizure
- Haemorrhage
- Venous ischaemia
- If symptomatic it will be due to
- Increased inflow,
- Compromised venous outflow, or
- Remote arteriovenous shunt with increased venous pressure
- Haemorrhage may occur but this is usually due to an associated CCM
- If a DVA diagnosed during investigation of intracerebral haemorrhage (ICH), one should exclude an associated CCM.
Pathogenesis
- An intrauterine ischaemic event during the formation of medullary veins (deep veins of the brain)—> collateral venous drainage
- DVAs are thought to develop in compensatory response to incidents during embryogenesis, thereby recruiting and dilating pre-existing transmedullary veins
Pathology
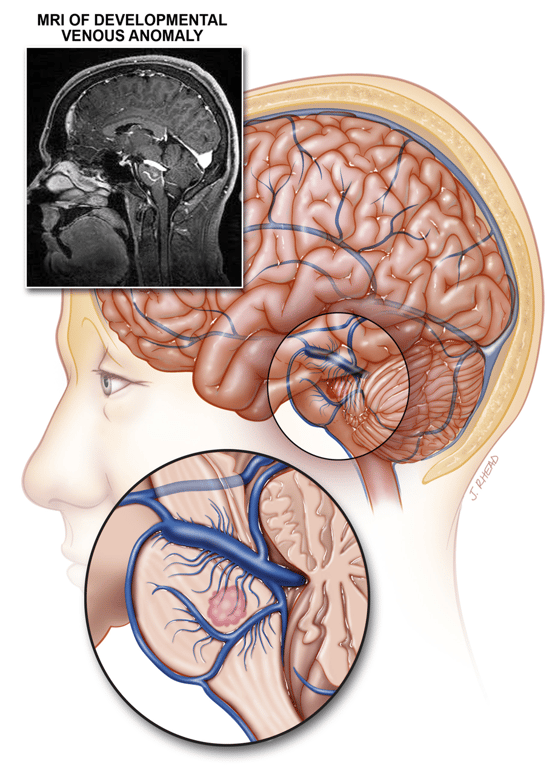
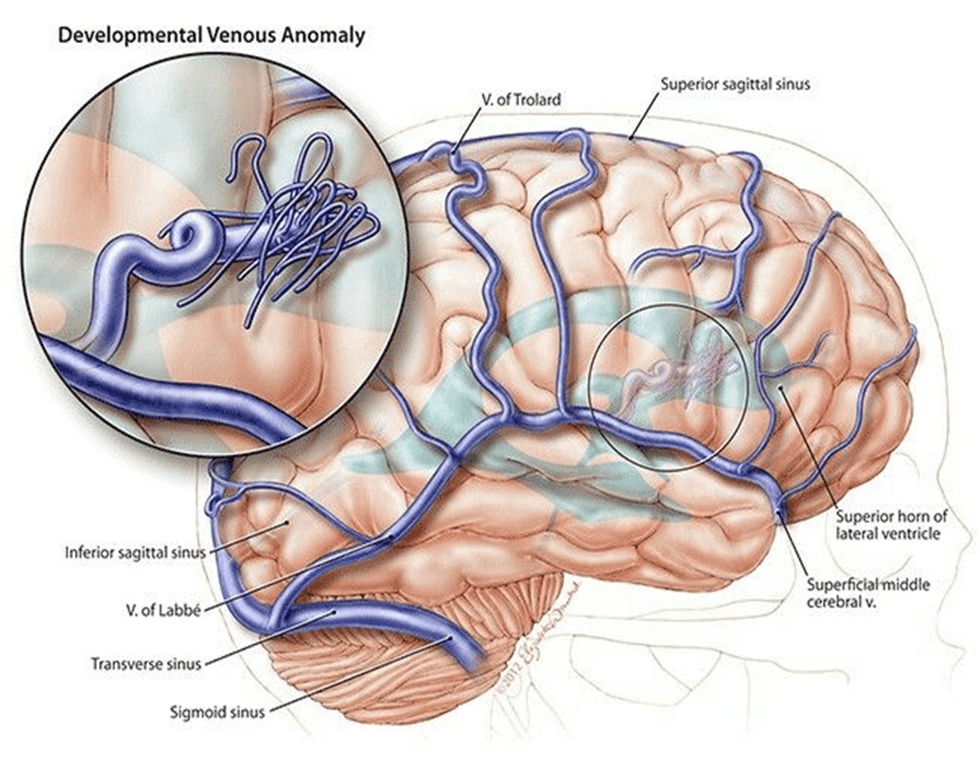
- Tuft of medullary veins that converge into an enlarged central trunk that drains to deep or superficial venous system
- Veins lack smooth muscle and elastin
- Normal arteries
- Presence of neural parenchyma between vessels
- Low flow, low pressure
Location
- Regions of MCA
- Vein of Galen
Imaging
- CT and MRI
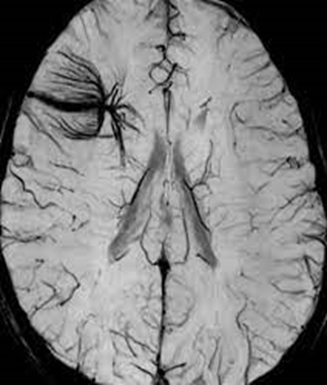
- Curvilinear enhancing structure or flow void with enhancement of the dilated medullary veins (‘caput medusae’).
- MRI: T2 hyperintensity on flair
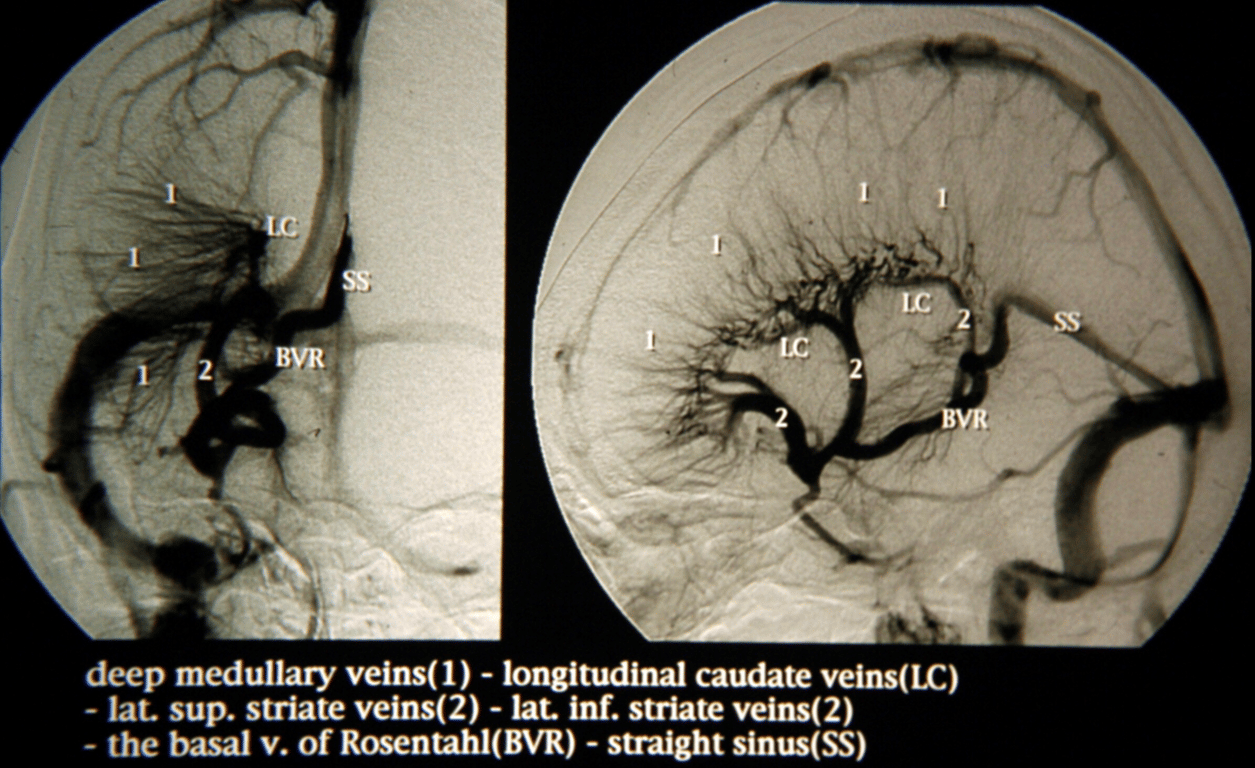
- Angiogram
- Can be angiographically occult
- The venous phase of angiogram demonstrates the caput medusae aspect of transmedullary veins draining into the venous collector vein, which in turn drains into either the superficial or deep venous system
Treatment
- In most patients, DVAs are normal variants that do not require treatment.
- Do not tx because of intervening brain tissue
- Indication for treatment:
- Documented bleeding DUE to angiomas
- Intractable seizures Due to cavernomas