Definition
- A rare, congenital neurocutaneous disorder involving the brain, skin & eye,
General
- AKA
- Encephalotrigeminal angiomatosis
- Encephalofacial angiomatoosis
- Rare sporadic disease
Genetics
- Most cases are sporadic
- Somatic mutation in a nucleotide transition in the gene GNAQ (Guanine nucleotide-binding protein G(q) subunit alpha) on chromosome 9q21 that occurs early after conception during in utero development.
Pathology
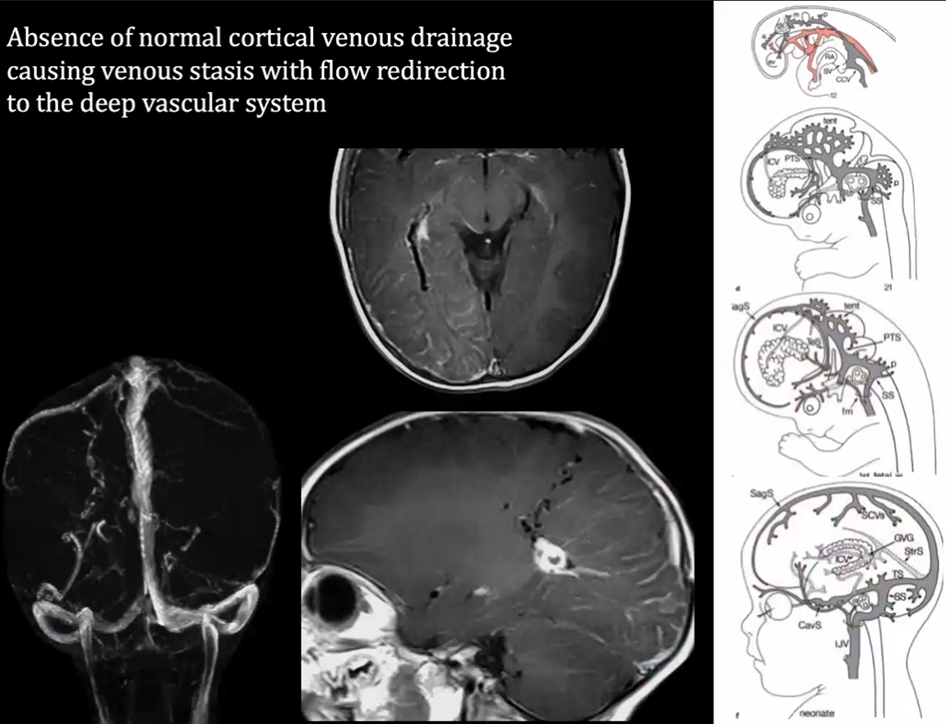
- Failure of the primitive cephalic venous plexus to regress in the first trimester
Diagnostic criteria
- 2 out of 3 of the following:
- Facial port-wine birthmark (facial angiomas)
- Increased intraocular pressure
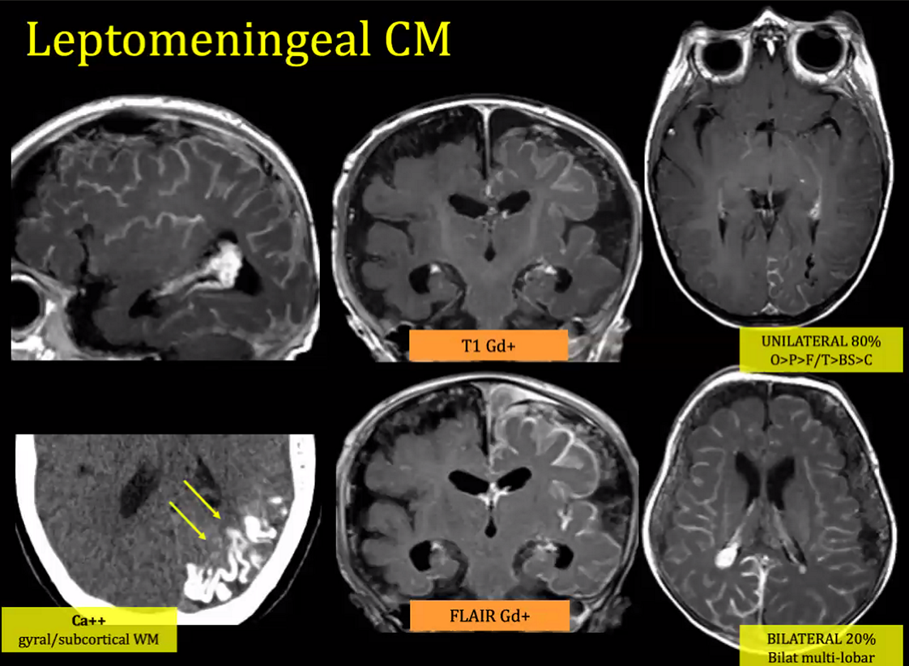
- leptomeningeal angiomatosis
- Patients with only leptomeningeal angiomatosis and no skin or eye involvement are considered to have the intracranial variant of SWS.

Subtypes (Roach scale)
- Type 1: Leptomeningeal plus facial +/- Glaucoma
- Type 2: facial only +/- Glaucoma
- Type 3: leptomeningeal only
Clinical features
- Cardinal features:
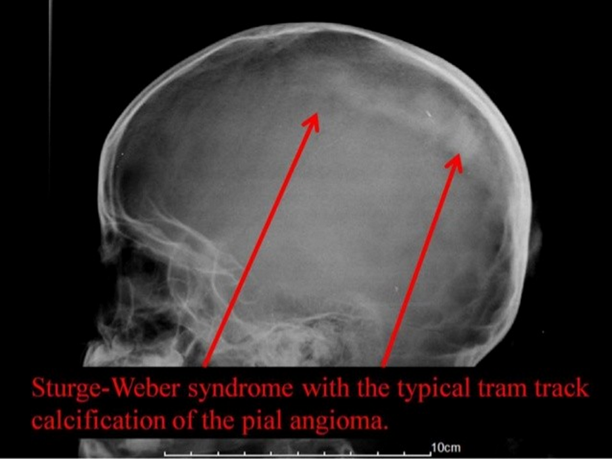
- Localized cerebral cortical atrophy and calcifications (especially cortical layers 2 and 3, with a predilection for the occipital lobes):
- Calcifications appear as curvilinear double parallel lines (“tram-tracking”) on plain X-rays
- Cortical atrophy usually causes contralateral hemiparesis, hemiatrophy, and homonymous hemianopia (with occipital lobe involvement)
- Ipsilateral port-wine facial nevus (nevus flammeus) usually @ V1 (forehead and/or eyelid) (rarely bilateral):
- Not always present, alternatively sometimes in V2 or V3 regions
- 8–20% of patients with facial port-wine birthmarks (with or without ocular involvement) develop neurologic symptoms.
- Risk of SWS symptoms
- port-wine stain only in V2 and V3 have a lower risk
- bilateral V1 birthmarks have a higher risk (≈ 35%)
- Other findings
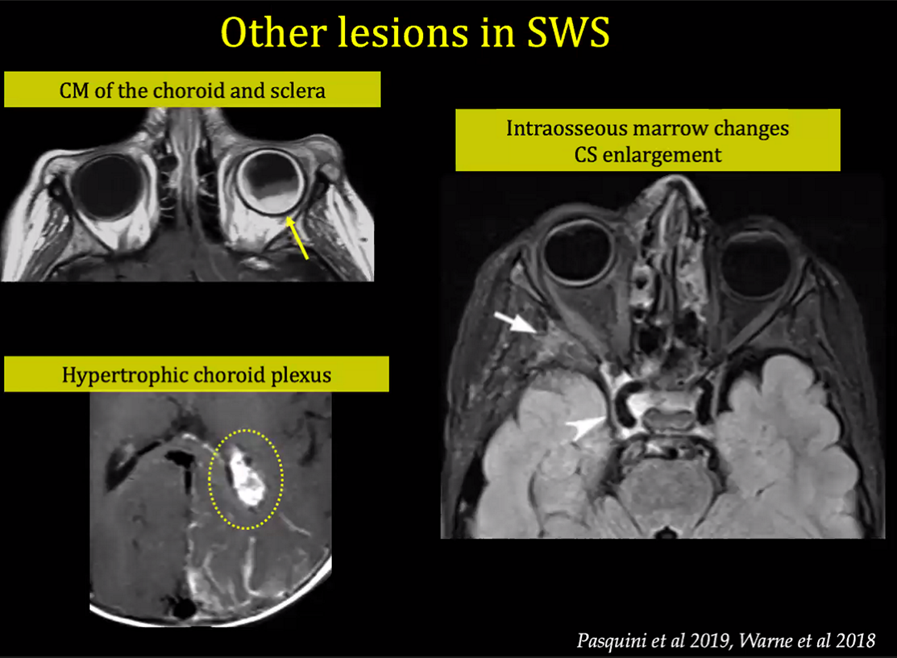
- Ocular involvement
- Occurs in around 60%
- Glaucoma
- most frequent ocular finding
- may present at any time between birth and the fourth decade.
- May be unilateral or bilateral, with the latter being more common in patients with bilateral facial PWS.
- Due to
- Vascular malformations of the eye in patients with SWS may involve the conjunctiva, episclera, choroid, and retina.
- Oculomeningeal capillary haemangioma
- Retinal angiomas
- Other eye findings include
- Nevus of Ota
- Buphthalmos
- Blindness
- Coloboma of the iris
- Neurological deficit
- Hemiatrophy (possibly from chronic cerebral hypoxia)
- Progressive hemiparesis 30%,
- Hemianopsia (40-45%)
- Seizures
- Seizures in 1 st year of life (dev. delay)
- by the age of 5 years: 95%
- contralateral to the facial nevus and cortical atrophy.
- Present in most patients starting in infancy
- Mental retardation or learning disability (50-75%)
- Migraine like headache (the prevalence in children of < 10 years of age is significantly higher than the general population at 31 versus 5%, respectively)
- Moyamoya disease
- Arteriovenous malformation of the lung and liver
- Endocrinopathies:
- GH deficiency is more common
- (18-fold general population)
- For suspected or confirmed SWS, screen for this in children ≥age 2 years by measuring serum IGF-1
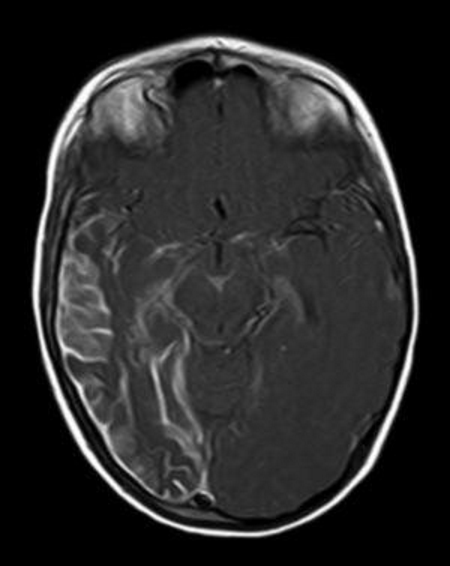
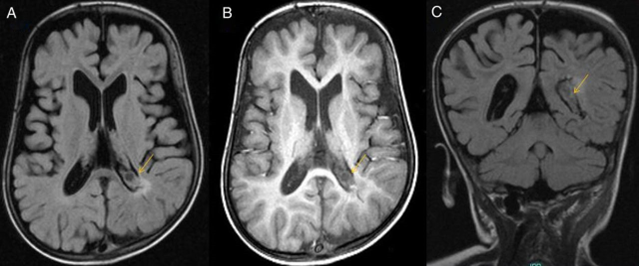
- Arrow showing enlargement of the choroid plexus,
- Atrophy of the occipital lobe
Treatment
- General
- Treatment is supportive.
- Aggressive management of fever
- Flu vaccine
- Headache: symptomatic treatment
- Seizures:
- frequent and protracted seizures exacerbate the neurologic damage.
- Aim early aggressive treatment of seizures
- first-line treatment: anticonvulsants
- oxcarbazepine
- common initial drug.
- Side effects include central hypothyroidism, especially in girls
- levetiracetam &
- topiramate
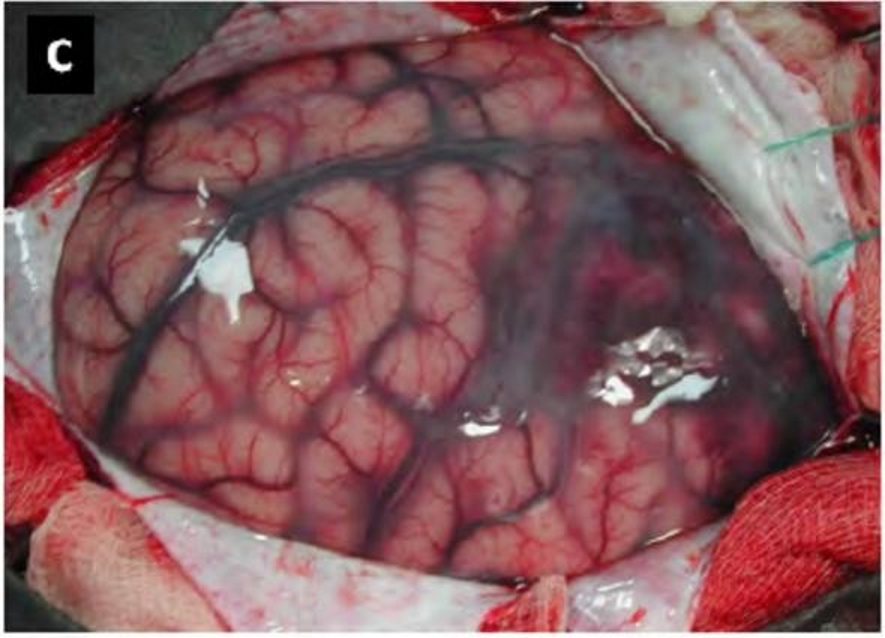
- 2nd line: lobectomy or hemispherectomy
- For refractory seizures
- Options include:
- Functional hemispherectomy
- Anatomic hemispherectomy
- Stroke prevention (aspirin, good hydration)
- Glaucoma: annual ophthalmology check
- Facial angioma: dermatology referral
- Skin lesions:
- laser treatment (currently, flash lamp-pumped PDL is favoured) can lighten the birthmark.
- May also reduce hypertrophy of soft and bony tissue.
- Endocrinopathies:
- Monitor growth and thyroid function
- Growth hormone deficiency can be replaced; however, there may be a risk of increasing seizures.
- XRT: complications are common and benefits are lacking.